The anterior spinal syndrome is one of common complications of spinal shock. However, to talk about what neurological symptoms will be present after the signs of shock disappear, just can not say – it takes some time.
Symptoms
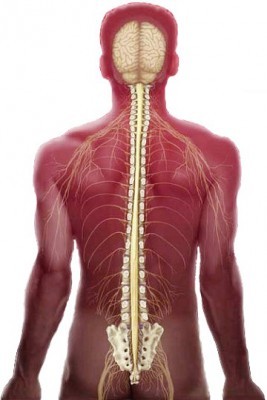
Spinal shock is one of the most serious diseases characterized by disorders of motor, sensory and reflex functions of the spinal cord. It happens only at the level below the affected places. This condition develops fairly quickly, and sometimes it takes a few hours, in rare cases, several days, and rarely weeks.
The main clinical manifestations of this condition on the part of the autonomic nervous system should be considered as slowing heart rate, lower blood pressure and decrease in body temperature. Another important clinical sign, which may further cause anterior spinal syndrome is a disturbance of the gastrointestinal tract.
During the shock to assess how badly damaged the nervous system, and what to expect as consequences, is impossible. And why exactly is this disorder, to tell difficult. Many authors who have studied it in some detail, noted the reasons for its development.
The most profound and prolonged shock of this kind arises in the case of anatomical gap spinal column. While there is full body paralysis below the site of interruption of the brain and a complete violation of all kinds of sensitivity and functions. But nothing complicated shape can last from 15 to 20 days. But clinical studies have shown that this time can be greatly stretched, and the majority of patients emerge from this state not earlier than after 4 to 8 weeks after injury. The symptoms can not only go, but to grow, for example, in the presence of a hematoma or of fragments of bones of the vertebrae, which will squeeze the brain.
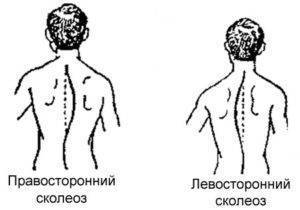
Classification
The degree of violation of the spinal column, all types of injuries can be divided into several categories:
- Full damage, where there are no motor and sensory functions.
- Incomplete – while motor function is maintained above the fracture site and is completely absent below it.
- Incomplete – motor function remains below the affected space and muscle power in this case reaches only 3 points.
- Incomplete when motor function is preserved below the injury, muscle strength of 3 points or more.
- There is no damage. Here all features are retained fully.
Diagnosis
It is important to conduct timely diagnosis and to learn to distinguish a shock from another, less common after a trauma condition, which is called autonomna dysreflexia.
In this case, the symptoms are as follows:
- High blood pressure.
- The low heart rate.
- Headache that is throbbing in nature.
- Alarm.
- Sweating of the skin.
- Pain in the abdomen.
Dysreflexia treated for 2 to 4 days, and this is done symptomatically.
Complications
After the main phenomena regress, there is a period of residual phenomena. And here, in the foreground is a complication as a failure of the ventral half of the spinal cord. It happens only in the case of partial damage. This may also include the posterior spinal syndrome, centripetally sinram, cauda equina syndrome brown-sekara.

The anterior spinal syndrome is the result of hyperflexion damage. This happens most often in road traffic accidents or when diving head down. It is accompanied by disorders of the spinal cord. Basically, this type of injury occurs in the neck, or to be more precise – from 3 to 7 cervical vertebrae. In addition to the compression fracture may dislocation of the vertebrae. As a manifestation of spinal injury is relatively rare and the main reason we should consider all the same car accident.
Treatment
Since pathology is a consequence of the shock, the treatment will be quite lengthy, and to cure this condition completely almost never fails. It is important that patients with such a diagnosis, like spinal cord injuries receive proper care and correct treatment. Equally important is the rehabilitation that needs to take place almost immediately after the incident – first on the healthy limb, and after treatment and on the affected side.