Hepatic coma – severe oppression of the functions of the Central nervous system, which occurs due to liver failure.
It is an urgent condition that requires not just medical assistance, and immediate action – otherwise, the patient will not survive.
When liver failure (depression of all the functions of the liver, which develop on the background of many of its diseases), hepatic coma does not occur immediately.
Precedes hepatic encephalopathy – a violation on the part of the brain that occur due to severe liver disease and, as a consequence, formation of toxic products that cause destruction (destruction) of nerve cells.
General data
Hepatic coma is one of the most severe emergency conditions. This is a disease that can hardly be corrected, and often lethal even against competent intensive therapy in conditions of high diagnostic and therapeutic support.

Severe impairment of the brain occurs in 30% of all patients with liver failure, transformed in a coma.
Reasons
The immediate cause of hepatic coma is decompensated liver disease, which violated many of its functions. It is often chronic liver disease, although acute onset destructive violations also can result in liver failure and coma.
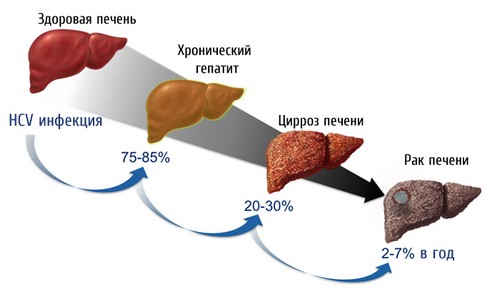
Most often disease, provoking the development of hepatic coma, may be the following pathology:
- a number of cirrhosis – primary biliary, viral, alcoholic, toxic, stagnant;
- various forms of hepatitis – viral, alcoholic, steatohepatitis (deposition of fat particles in the liver), autoimmune, drug;
- different types of hepatosis of liver lesions and non-neoplastic non-inflammatory nature, characterized by metabolic disorders in the liver cells. Most often it is pigmented, the acute and chronic fat, chronic cholestatic (bile stasis) steatosis, acute toxic dystrophy of the liver;
- malignancy – gepatozellliarnaya carcinoma, cholangiocarcinoma, hepatoblastoma, mixed with cancer;
- inherited disease – hemochromatosis (iron deposition in liver cells), the disease Konovalov-Wilson (accumulation of copper in liver tissue), Gilbert syndrome (deposition in the hepatocytes of the pigment lipofuscin, also known as pigment wear).

In most cases, hepatic coma occurs not just in the background of such diseases and impairment of their flow – the reason is the so-called breakdown of compensation provocateur which, in turn, can be:
- gastrointestinal bleeding (chronic and acute);
- prolonged alcohol experience;
- diffuse peritonitis (especially purulent);
- sepsis of the body;
- anesthesia using halothane of the drug;
- chronic intestinal obstruction due to various pathologies of the large intestine;
- for a long abdominal surgery under endotracheal anesthesia;
- administration of various drugs – most commonly sedatives (sedatives), narcotic and non-narcotic analgesics, anti-TB drugs from all three classes of efficiency, diuretics (diuretics).
Less frequently hepatic coma occurs in the background of the so-called fulminant liver failure – that is, such, which, in turn, can develop suddenly, without previous liver disease.
This is quite a rare disease, mostly occurs in such diseases and conditions as:
- hepatotoxic effect (i.e., precisely what influence on the liver cells) poisons – it might be poisoning inedible mushrooms, alcohol (counterfeit or plain, but in high doses), nitrates, pesticides, industrial poisons;
- severe infectious diseases – as non-specific (influenza, parainfluenza), and specific (tuberculosis);
- intraoperative shock – hemorrhagic (loss of blood), pain.
In 17% of all clinical cases of causes of hepatic coma remains unknown.
Development status
Hepatic coma is a terminal (final) stage of brain damage (encephalopathy). From the point of view of biochemical processes important mechanism is the destruction (damage) of brain cells due to exposure to endogenous toxins (i.e., produced by the body as a result of failures in its activities).
Most often these are substances with toxic properties, such as:
- ammonia;
- fatty acids;
- phenols.
Obrazujas in the large intestine, ammonia enters the portal vein and the vessel enters the hepatocyte – but, contrary to expectations, is not included in the normal cycle of processing and disposal (the so-called ornithology cycle). The rate of physiological reactions of ammonia is greatly reduced, and toxic products that are produced at different stages of its processing, begin to enter into the General circulation.
These toxins affect between themselves and “strengthen” each other – as a result:
- increases their penetration through the blood-brain barrier (a physiological barrier, which normally protects the brain cells from getting here and the impact accidentally entered the bloodstream of toxic substances);
- disturbed water-salt regulation inside brain cells.
Such factors (especially water-salt failure) lead to accumulation of fluid in the brain cells. There is swelling of brain tissue.
The harmful effects of toxins on the cells of the brain, resulting from failure of the liver, is also the next they’re:
- breaking the sequence of energy processes in the nerve cells;
- reduce the speed of processing glucose, without which brain tissue can’t digest;
- provoke oxygen starvation of neurons.
All three of these processes not only themselves are harmful to brain cells but also increase its swelling, thus, each causing a double impact on neurons.
The most negative consequence of cerebral edema – the scheduling of its trunk (shifting between other structures or in the foramen Magnum, resulting in intense pressure and critical breach of its viability).
The wedging of the brain stem is the main cause of death in 82% of all clinical cases of hepatic coma.
The symptoms of hepatic coma
The basis of the clinic of hepatic coma are:
- neuropsychiatric symptoms – the symptoms of Central and peripheral nervous system;
- signs of actual liver failure.
Clinical manifestations of hepatic coma depends on its stage.
There are two stages of this condition is:
- shallow (or initial);
- deep.

During shallow stages of hepatic coma determine such neuropsychiatric symptoms:
- consciousness is absent;
- retained reactions to painful stimuli (pinching, injections);
- the saved reflexes such as gag (a gag motions when any subject of irritation of the posterior pharyngeal wall) and corneal (the closing of the eyelids in response to stimulation of the cornea);
- pupils dilated, their reaction to light is weakened;
- possibly involuntary urination and defecation (emptying the rectum);
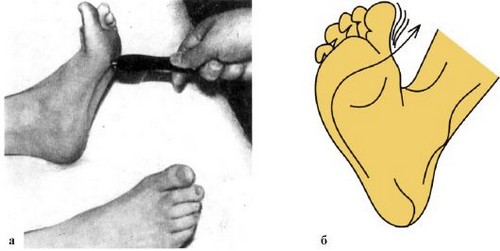
- fixed pathological reflexes – Zhukovsky (neurological hammer to easily tap the middle portion of the plantar surface just below the toes in response to irritation of the fingers from the second to the fifth bend involuntarily), Babinski (skin the outer edge of the sole annoying, making the bar touch, in response to the irritation of the first toe to bend), and others;
- there are cramps;
- is determined by the so-called decerebration rigidity of the limbs – hands and legs of the patient like a wood, do not bend or difficult to bend in the joints;
- despite the fact that patients are unconscious, some of which are small movements – grasping, chewing.
During the deep stages of hepatic coma determine such neuropsychiatric symptoms:
- the patient does not have any reaction to any stimuli pain (tingling, injections), temperature (applying to the skin a cold or hot object), olfactory (a present to nose fleece with ammonia);
- there is an absolute areflexia (absence of reflexes). Including not occur corneal reflex and pupillary response of the patient to directed the beam of light;
- palsy (insolvency) of the sphincter of the bladder and rectum occur involuntary urination and defecation;
- often there may be generalized (widespread) clonic seizures (involuntary twitching of muscles and individual muscle fibers due to the change in muscle tone).
Signs of liver failure occur at all stages of hepatic coma.
The most common are the following:
- skin, sclera and visible mucous membranes are icteric hue;
- mouth the patient feels the typical liver smell – sugary and sweet;
- observed a hemorrhagic syndrome – possible gastro-intestinal, uterine, nasal bleeding, petechial hemorrhages in skin and mucous membranes;
- the heart rate is increased;
- blood pressure is lowered;
- the body temperature is elevated.
The apogee of advanced stage hepatic stage – respiratory arrest (particularly because of the defeat of the respiratory center).

In addition to the cerebral edema, the most common causes of death can be:
- generalized infectious complications, sepsis of the body and, as a consequence, infectious-toxic shock (depression of brain activity toxic products that can not neutralize the affected liver);
- kidney failure;
- pronounced necrosis of liver tissue, which leads to a twofold effect – a dramatic inhibition of liver function and toxic effects on the brain products of necrosis of hepatic tissue;
- pulmonary edema.
Diagnosis
Signs of coma, quite characteristic. The task of physicians to determine that it is of hepatic origin. Confirmation of the diagnosis possible on the basis of clinical symptoms, chronic liver disease in the anamnesis.
Have value details of history to find out the relatives of the patient:
- in some of the disease or condition arose pathology;
- when the first symptoms;
- as rapidly developed signs of disease.
To confirm the diagnosis and assess the degree of disorders of the liver and brain used additional diagnostic methods – physical, instrumental and laboratory.
Data of physical examination is quite similar to many species of whom (except for some nuances):
- during the inspection, they fixed the lack of consciousness of the patient, the skin, sclera and visible mucous membranes are icteric;
- the patient does not respond to palpation (probing) of the anterior abdominal wall, the voltage is not detected;
- percussion uninformative;
- auscultation weakened peristalsis (due to associated toxic shock bowel the toxic waste products of the body that are not neutralized, because the liver is incapable).
Instrumental methods that are used in this pathology, the following:
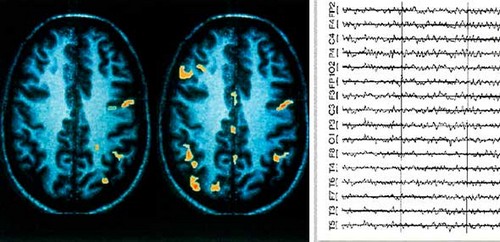
- electroencephalography – in the case of hepatic coma on the EEG reveals slowing or complete absence of alpha rhythms, as well as the predominance of theta and Delta waves;
- computed tomography of the brain (CT) – computer sections investigate and evaluate the foci of changes within the brain and the degree of its destruction;
- magnetic resonance spectroscopy of the brain – using this method is to measure the prevalence of metabolites (products of biochemical reactions) in the brain.
Also in the diagnosis of hepatic coma used laboratory methods is:
- General analysis of blood – signs of anemia (reduction of haemoglobin) and the increase in the number of platelets;
- biochemical analysis of blood – it has noted an increase in the amount of bilirubin, a significant increase in the activity of serum transaminases, the decrease of the number of common protein;
- coagulation – there is a decrease in prothrombin index;
- analysis of the cerebrospinal fluid – it is determined by an increased amount of protein;
- Toxicological examination of blood – detection in the blood of toxic compounds;
- a blood test for the presence of markers of viral hepatitis.
Differential diagnosis of
Differential (distinctive) diagnosis of hepatic coma should be carried out with such pathological conditions as:
- acute disorders of cerebral circulation (ischemic and hemorrhagic);
- coma metabolic disorders – most often seen in hypokalemia (decrease of potassium in the serum of the blood), uremia (excess of nitrogenous substances in the blood);
- terminal (final) stage toxic encephalopathy (brain damage of various poisons).
Treatment and first aid in hepatic coma
Patients with hepatic coma urgently hospitalitynet in the intensive care unit and intensive care and begin the constant:
- ECG-monitoring (the continuous monitoring of electrical activity of the heart);
- the pulse oximetry – the determination of the degree of blood oxygen saturation;
- control of intracranial pressure.
Treatment – intensive conservative therapy. It is based on such assignments as:
- the fastest possible identification of the factor triggering the occurrence of hepatic coma (gastrointestinal bleeding, infections, mushroom poisoning, alcohol, or industrial poisons, and so forth) and its liquidation;
- intubation and connection to the apparatus of artificial lung ventilation (ALV). Is due to the fact that in hepatic coma, and there is growing respiratory failure;
- deep sedation – the administration of drugs, which support neurons in the “relaxed” state. For this purpose, fentanyl and propofol;
- to meet the shortage of blood glucose and correction of oxygen deficiency of brain neurons intravenously administered glucose solution;
- when bleeding and change of indicators of blood coagulation fresh frozen plasma is administered intravenously;
- by reducing the amount of hemoglobin below 70 g/l carry out the transfusion of whole blood;
- by reducing the amount of proteins in the blood administered intravenously protein drugs;
- to prevent infectious complications (including artificial ventilation) used antibacterial drugs;
- for reducing the absorption of ammonia in the intestine and toxic destruction (damage) of neurons in the brain administered lactulose;
- for the prevention of gastrointestinal bleeding with use potassium supplements, proton pump inhibitors.
It should be remembered that in hepatic coma possible stress destruction (destruction) of the mucous membrane of the digestive tract, including fraught bleeding.
- to enhance the enzyme activity in the liver cells, muscles and brain are attracted to medicines L-ornithine-L-aspartate;
- to facilitate bowel movements put regular enema with a solution of magnesium sulfate or siphon enema;
- to enhance the stability of liver cells to toxic substances, as well as for speeding up (accelerating) processes of regeneration (restoration) administered arginine glutamate, preparations of milk Thistle, thiotriazolin and others;
- for the purpose of detoxification is carried out extracorporally detox. It will perform using hemosorption (blood sampling from the blood stream, cleanup and return it to the bloodstream) or hemodialysis (blood purification using the apparatus “artificial kidney”).
If several hours have significantly worsened neurological symptoms should be suspected increased intracranial pressure.
In doing so:
- artificial lung ventilation (ALV);
- sedation;
- normalization of body temperature;
- correction of electrolyte and gas composition of blood.
If the application of these methods is not observed properly or no effect is carried out:
- hyperosmolar therapy for this intravenously administered mannitol, hypertonicity solution of sodium chloride;
- hyperventilation (increased ventilation of the lungs). Forced ventilation will reduce intracranial pressure for 1-2 hours, during this period of time, undertake other activities;
- moderate cooling of the body of the patient.
In extreme cases perform a decompressive craniotomy – surgical intervention, during which conduct examinations of the skull to reduce intracranial pressure.
Patients who are in hepatic coma, fed through parenteral method is intravenous drip-feed of nutrients, and the calories must be saved, but the amount of protein is reduced.
The only method with high efficiency in the case of end-stage liver failure and hepatic coma – transplantation (transplantation) of the liver.
Prevention
The main prevention of hepatic coma on the following activities:
- timely detection and treatment of liver diseases – cirrhosis (especially viral), hepatitis, cancer and others;
- the prohibition of self-medication by patients with hepatic symptoms, even slightly severe;
- competent selection and appointment of drugs;
- measures that will help to avoid poisoning any poisons – production of toxic substances, mushrooms, household tools and so on;
- the refusal of alcoholic beverages.
Also, when pre-existing liver disease, special attention should be given to diseases and conditions that can trigger rapid onset of hepatic encephalopathy and its consequences – hepatic coma.
In the first place is:
- bleeding of the digestive tract;
- the intake of alcohol;
- severe infections of the body – in particular, with the development of sepsis;
- bowel disease, which may develop intestinal obstruction;
- the need for surgical intervention on organs of the thoracic and abdominal cavity;
- the necessity of taking certain groups of drugs – especially sedatives and anti-TB.
Forecast
The prognosis of hepatic coma extremely unfavorable, the risk of death is very high – survival of less than 20% of all patients.
The highest mortality (deaths) observed in such conditions as:
- before age 10 and after age 40;
- duration of jaundice period of less than seven days before the development of signs of severe encephalopathy;
- the amount of bilirubin in the blood of more than 300 µmol/l;
- rapidly increasing changes in the liver, which lead to its reduction;
- joining the infectious agent;
- severe degree of respiratory failure.




Its like you read my mind! You appear to know so much about this, like you wrote the book in it or something. I think that you can do with some pics to drive the message home a bit, but instead of that, this is fantastic blog. A great read. I’ll certainly be back.