Viral hepatitis in pregnant women – a group of infectious diseases with primary damage to hepatic tissue, caused by hepatotropic viruses and detected during gestation.
Manifested severe intoxication, jaundice, dyspepsia, change in the color of urine and feces, enlargement of the liver.
Diagnosed with IFA, RIF, PCR, laboratory studies of enzyme systems, pigment, protein, fat metabolism, supplemented by General blood test and ultrasound results of the liver. For treatment using infusion therapy, hepatoprotectors, choleretic agents in combination with health-protective regime and diet.
Viral hepatitis in pregnant women
Viral hepatitis detected in the 0.2-3.0% of pregnant women in 40-70% of cases of jaundice during gestation is caused by viruses. More than alf of the patients diagnosed viral hepatitis B, acute form of the disease occurs with a frequency of 1-2 cases per 1000 pregnancies, chronic – 5-15 per 1000.
The second most common is hepatitis A, the third, which is increasingly found in the period of carrying a child. As a result of researches it is established that, under equal conditions, pregnant, trapped in the focus of infection, get sick 5 times more often than other entities. risk Factors are young age, low incomes, poor physical living conditions, promiscuous, living in epidemicus adverse countries with low availability of quality medical care.

Causes of viral hepatitis in pregnant women
The etiology of liver hepatotropic viruses in the gestational period is the same as in other cases. Agents of the disease become RNA – and DNA-containing viruses of different types A (HAV), B (HBV), C (HCV), D (HDV), E (HEV). In recent years, experts in the field of infectious diseases have reported a possible role in the development of the hepatitis viruses F, G, SEN V, TTV, etc. pregnant women are increasingly diagnosed mixed hepatitis, which provoked several pathogens and often occur heavier. There are several risk factors that increase the probability of infection during pregnancy.
Their role increases significantly when poor hygiene, asepsis, antiseptics:
- Stay in a medical facility. Pregnant hospitalitynet to the hospital before the birth, in the event of obstetric complications, presence of severe extragenital pathology. In the territories and in countries where there are problems with hygiene and sanitation, possible fecal-oral contamination of the patient with viral hepatitis A, E, and even the occurrence of hospital-acquired epidemics.
- Performing invasive manipulations. In violation of the rules of asepsis and antisepsis serious problem is the risk of infection with hepatotropic viruses with parenteral transmission. Pregnant can become infected while using contaminated instruments, installation of droppers, applying forceps, performing invasive prenatal studies, and surgical interventions.
- Blood transfusion. There are a number of conditions requiring blood transfusion and its components. Transfusion therapy is prescribed in case of massive bleeding, DIC-syndrome, severe anemia, hemorrhagic shock, postpartum sepsis. Although careful quality control of blood, minimizes such risks, infection is possible in case of emergency when working with untested donors
Pathogenesis
The mechanism of development of pathological process depends on the characteristics of pathogens. Most viral inflammation of the liver, severe anthropology, but the virus natural reservoir of HEV can be pigs and rodents. The incubation period is 15-50 days hepatitis A and C, 20-80 days when infected by hepatitis D, E and 40-120 days in hepatitis type B.
In the case of infections of the alimentary and water transfers entrance gate is the mucosa of the gastrointestinal tract, after which the viral agent is replicated in mesenteric lymph nodes and vascular endothelium of the small intestine. Through the blood the pathogen spreads throughout the body, which is clinically manifested intoxication syndrome, then goes to the liver. Through sexual, parenteral, and vertical mechanisms of transmission of pathogenic agent immediately gets into the blood stream and then via the blood to the liver.
All types of hepatotropic viruses except HBV serotypes, have a direct cytopathic effect and cause cytolysis of hepatocytes. Damaging factor in the development of viral hepatitis B is amplified immune response with inflammation and necrobiotic processes. For replication of the virus HDV requires the virus-assistant, which is the causative agent of hepatitis B. a pregnant woman develops clinical and laboratory signs of cytolytic, cholestatic, expressed mesenchymal-inflammatory biochemical symptom. The causative agents of hepatitis A and E from the destroyed liver cells go to the bile and then excreted into the environment, polluting it. The viruses HBV, HCV and HDV continue to circulate in the blood.
Solimine of the pathogen due to the high immunogenicity happens when infected by pathogens hepatitis B (normal immune response), A, E. HDV are eliminated after the disappearance of HBV, without which there is no further replication of the virus. Because of the high rate of mutation of the causative agent of hepatitis C is low in immunogenicity because of the chronic progressive course of the disease. The chronic disease is also possible with a weak immune response to the virus HBV, mutations of the pathogen, integration of viral DNA into the genetic apparatus of hepatocytes, lack of synthesis of α-interferon, the occurrence of autoimmune reactions.
Classification
Systematization of the forms of viral hepatitis in pregnant women is based on the same criteria as outside of the gestational period. According to the severity of the clinical manifestations are subclinical, light, medium, heavy, fulminant (fulminant) viral infection of hepatocytes. In the course of the disorder can be acute, protracted, chronic. The highest value for a choice of medical tactics plays a classification according to the mechanism of transmission.
Infectious diseases are distinguished:
- Hepatitis with fecal-oral infection. This group includes infectious processes caused by viruses HAV, HEV. The incidence of hepatitis a (Botkin’s disease) is up to 1/3 of all cases of infection of pregnant women. Hepatitis E is an endemic disease, detected primarily in the developing countries of Asia (India, Burma, etc.). Such viral liver disease is not passed from mother to fetus.
- Hepatitis with blood-contact infection. Injecting, sexual, vertical intrusion method characteristic of infections caused by viruses HBV, HCV, HDV. Diseases of this group may occur as acutely and chronically, causing gross destructive changes of liver tissue. When administered to a pregnant it is important to consider the possibility of infection of the fetus and to carry out the prevention (vaccine, etc.).
Symptoms of viral hepatitis in pregnant women
In the classical acute course in infected strains of viruses HAV, HBV, HDV, HEV, after an incubation period signs of intoxication syndrome with hyperthermia, arthralgia, weakness, fatigue, rapid fatigue, sleep disorders. Possible dyspeptic symptoms as nausea, decrease or lack of appetite, rarely vomiting. There is a heaviness, mild swelling in the right hypochondrium, the epigastric region. 20-30% of pregnant same feelings are marked in the left hypochondrium due to the increase of the spleen. A few days after the appearance of prodromal symptoms, the urine becomes brown or brown, discolored feces, the color and texture of which remind white (grey) clay. Djelturanga the duration of period ranges from 3-10 days to 1 month depending on features of the pathogen, in some cases, this period is missing.
On the onset of the icteric period, usually lasting from 1 to 3 weeks, the staining shows in yellow color the skin and visible mucous membranes. While pregnant women suffering from hepatitis A, there is an overall improvement of health. For hepatitis E, B, D intoxication may increase. The formation of cholestasis is accompanied by the appearance of pruritus. The duration of the recovery period for different types of viral liver damage ranging from several months to a year. Possible erased and Busselton the course of the disease with minimal symptoms and a quick recovery.
In women with hepatitis C clear clinical picture usually absent, sometimes the infection becomes accidental discovery in a laboratory screening. In most cases, once the disease takes a chronic nature with periodic worsening liver tests and progressive development of extrahepatic autoimmune disorders (with the defeat of the thyroid gland, kidneys, blood vessels, joints, bone marrow, etc.).
Complications
Pregnancy usually complicates the course of hepatitis, especially caused by the virus HEV. The worsening of symptoms with the development of cholestasis is more pronounced after the 20th week of gestational period. In pregnant women infected in 3rd trimester, viral hepatitis E can occur with the occurrence of fulminant acute liver failure, progressive renal insufficiency, DIC-syndrome, premature birth, antenatal fetal death, stillbirth, developmental delays and severe hypoxia of the newborn. When fulminant for maternal mortality reaches 20-50%.
Toxic degeneration, submassive and massive necrosis of the liver functional failure, severe encephalopathy, hemorrhagic syndrome may complicate the course of acute hepatitis B and lead to the death of women. The mortality rate of pregnant women with this disease is 3 times higher than non-pregnant women. The chronic process with the growth of autoimmune disorders observed in 10-15% of patients with hepatitis B, 80% with hepatitis C, 50% – with hepatitis D. the long-term effects in the form of fibrosis, cirrhosis, malignancy with the formation of primary hepatocellular carcinomacancer for chronic disease.
Obstetric complications are usually observed in severe acute parenteral hepatitis and rarely with Botkin’s disease. My patients are 1.6 times more often compounded for gestosis, premature labour starts, there is premature rupture of membranes, possible preeclampsia during childbirth, the baby is born in a state of hypoxia with poor performance on a scale of Apgar. According to observations of gynecologists and obstetricians, all causative agents of viral liver lesions are not teratogenic. The causative agents of hepatitis B, C, rarely D can be transmitted from mother to fetus through the placenta, in childbirth, and through breastfeeding. The risk of infection ranges from isolated cases of infection with hepatitis D and 7-8% in hepatitis C, up to 80% with hepatitis B. the Figures are even greater for pregnant women with immunodeficiency (HIV infection, etc.).
Diagnosis
In the presence of epidemiological assumptions and classic symptoms, the diagnosis presents no special difficulties. Diagnostic difficulties are possible when oligosymptomatic, atypical for the reactivation of a chronic process. Given the high risk of infection of the fetus with the virus and chronic blood-contact all pregnant hepatitis, further laboratory screening.
The examination plan usually includes methods to identify the virus and evidence of hepatic dysfunction:
- Tests for verification of the pathogen. Specific ELISA markers of disorders are the corresponding total antibody Ig (M+G), antibodies to non-structural proteins (hepatitis C). DNA and RNA viruses can be identified using diagnostic PCR. RIF can detect virus particles in liver tissue, and other biological materials. In chronic hepatitis B and HBSAg carriers is determined.
- Liver function tests. A key marker of cytolysis of hepatocytes is at least 10-fold increase in ALT activity. The rate begins to increase since the end of the prodrome, reaches a maximum value at the peak and gradually reduces to normal during convalescence. Increasing the concentration of alkaline phosphatase (ALP) and gamma-glutamyltransferase (GGT) evidence of cholestasis.
- The study of protein metabolism. In inflammatory lesions of the liver parenchyma indicators sublimate samples are reduced, and thymol – are rising. The severity of the changes directly correlated with the severity of the infectious process. Reduced levels of total protein, albumin. It is noted dysproteinemia. Due to the violation of protein synthesis in the liver worsen the indicators of hemostasis system.
- Studying pigment and lipid metabolism. Functional failure of the liver is manifested by hyperbilirubinemia with predominant increase in the concentration of direct bilirubin, the presence in the urine of bile pigments and urobilinogen. Violation of the synthesis of cholesterol by hepatocytes, damaged in acute and chronic forms of viral hepatitis, accompanied by a drop in its level in the blood.
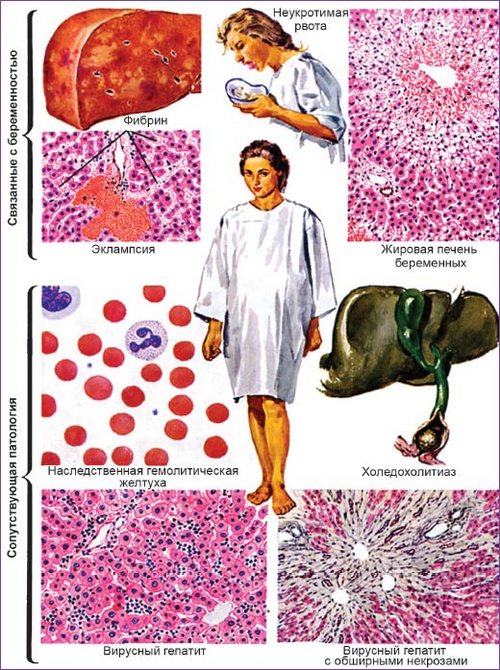
In General, the analysis of blood reduced the number of leukocytes, neutrophils, increased the relative content of monocytes and lymphocytes, erythrocyte sedimentation rate, often in the normal range, but can reach 23 mm/h. With ultrasound pechenocna revealed an increase in the size of the organ, in different variants of course possible hypoechoic, hyperechogenicity, heterogeneity of structure. Differential diagnosis is carried out between different variants of hepatitis. Infectious viral process also must be differentiated from lesions of the hepatic parenchyma in benign lymphoblasts, yersiniosis, leptospirosis, far East scarlet-like fever, drug hepatitis, severe early morning sickness, the pregnant cholestasis, pre-eclampsia, acute fatty hepatosis of pregnant women, HELLP syndrome. Except for the infectious disease patient according to indications consult a physician, hepatologist, dermatologist, neurologist, toxicologist.
Treatment of viral hepatitis in pregnant women
A woman with a confirmed diagnosis hospitalitynet in the infectious Department with obstetric wards. Termination of pregnancy via abortion is only possible in the early stages in the recovery period. Pregnant shown a sparing mode with the restriction of motor activity. Correction of the diet calls for the elimination of the alcohol, fatty, fried foods, eating a diet of meat (chicken, Turkey, rabbit), low-fat boiled, baked, steamed fish, cereals, dairy products, fresh vegetables and fruits. The amount of fluid intake is recommended to increase to 2 l/day or more. It is advisable to drink alkaline mineral water. In reconvalescence period shows limitation of physical activity, light diet.
Special etiotropic treatment options parenteral hepatitis in gestation is not performed. Pregnant women with severe disease, severe intoxication, serious disruption of liver functions recommended medicines with pathogenetic and symptomatic effects.
Given the symptoms, the treatment regimen may include the following groups of drugs:
- A means of detoxification. For elimination of toxic metabolites is used as a colloid, and crystalloid infusion solutions. Their purpose gives you the opportunity to stop the intoxication syndrome, to reduce the amount of itching caused by cholestasis, to improve rheological properties of blood.
- Hepatoprotectors. The use of phospholipids, botanicals, amino acids, multivitamin complexes, aimed at stabilizing cell membranes, protecting the hepatocytes from necrosis, tissue regeneration, improvement of biochemical parameters. They are usually prescribed for recovery.
- Choleretic and cholekinetic. Choleretic drugs are used when the threat or the occurrence of cholestasis. They allow to reduce the load on the hepatocytes, to facilitate the flow of bile, to remove its stagnation in the gall bladder, reduce the severity of the expressed mesenchymal-inflammatory changes in the liver.
When changes occur in the coagulation of blood regimen complement drugs that affect hemostasis. Pregnant women with extremely severe fulminant course, increasing liver failure was transferred to the intensive care unit for intensive therapy. The recommended method of delivery are natural physiological childbirth at term. Cesarean section is performed only in the presence of extragenital or obstetric indications (placenta previa, clinically and anatomically narrow pelvis, cross fetal position, tight obvity umbilical cord, pre-eclampsia).
Prognosis and prevention
With timely diagnosis in pregnant women with acute viral hepatitis and the correct choice of medical tactics, the pregnancy outcome is usually favorable. Maternal mortality does not exceed 0.4%, mortality due to severe extragenital pathology. The forecast becomes more serious when infected with the causative agent of viral hepatitis E in the 2nd half of pregnancy. In such cases, the risk of loss of the pregnant woman reaches 50%, in almost all cases the fetus dies. Options chronic disorders in gestation are activated very rarely. Preventive measures aimed at prevention, include personal hygiene and food hygiene, particularly when staying and visiting epidemiologically dangerous regions, refusal of unprotected sex, frequent change of sexual partners, injecting drug use, a careful study of donor materials, processing medinstrumenti.
To the viruses causing hepatitis A, E, B, formed persistent lifelong immunity. With the preventive purpose outside of pregnancy possible vaccination against hepatitis A, b and emergency immunization with immunoglobulins against HAV. Pregnant vaccines and serums prescribed with caution after studying all the possible indications and contraindications. Active-passive prophylaxis of infection of newborn blood-contact hepatitis can reduce the risk of infection by 5-10%. When viremia over 200 thousand IU/ml for women suffering from hepatitis B, antiviral treatment is prescribed nucleoside reverse transcriptase inhibitors, followed by active and passive immunization of the newborn.




I mastered more new things on this weight reduction issue. A single issue is that good nutrition is especially vital when dieting. A big reduction in fast foods, sugary food items, fried foods, sweet foods, red meat, and whitened flour products may perhaps be necessary. Retaining wastes parasites, and contaminants may prevent goals for fat-loss. While a number of drugs temporarily solve the challenge, the bad side effects aren’t worth it, plus they never offer you more than a non permanent solution. This can be a known incontrovertible fact that 95 of fad diet plans fail. Many thanks sharing your opinions on this blog.
Comodidad a su tramitar la eTA Canadá en línea.
Email Accuracy Validation through a premium industry level software process to determine if the emails are valid and accurate. Accuracy of between 95 and 97 Bring down your bounce rate on your mass email clients and decrease penalty’s.Lower the chance of your domain address being flagged as spam.
Thanks for expressing your ideas. I might also like to state that video games have been ever before evolving. Modern tools and innovative developments have made it easier to create reasonable and enjoyable games. These entertainment video games were not that sensible when the real concept was first of all being attempted. Just like other styles of technologies, video games also have had to progress via many decades. This is testimony towards fast growth and development of video games.
Hello there! This is my first visit to your blog! We are a collection of volunteers and starting a new initiative in a community in the same niche. Your blog provided us beneficial information to work on. You have done a wonderful job!
Do you have a spam issue on this site; I also am a blogger, and I was wondering your situation; many of us have developed some nice methods and we are looking to exchange techniques with other folks, why not shoot me an email if interested.