Hypophosphatasia (GF) is a rare genetic systemic disease caused by a mutation in a gene, which encodes tkanespecificescoe alkaline phosphatase (TSF) that leads to a deficiency of this enzyme and, consequently, to disturbances of mineralization of bone tissue.
In ICD-10 GF is identified with a code E 83.3. (Violation of exchange of phosphorus and phosphatase).
Heavy GF occurs in approximately 3.3 out of 1 million newborns 14. According to some, male newborns are more likely to suffer GF 7.
Inheritance
Childhood forms are inherited mainly in an autosomal recessive manner, the adult forms are inherited as autosomal recessive and autosomal dominant type. Autosomal recessive inheritance is associated with more severe forms of GF 1, 3. If the mutation is in the heterozygous state, then the bearer may be asymptomatic changes in laboratory parameters 3.
With autosomal dominant type of inheritance there is a 50% probability of pathogenic mutation variant. Prenatal diagnosis in pregnant women is possible if the pathogenic variant mutations were identified in a family member.

Etiology and pathogenesis
Alkaline phosphatase (ALP) is a membrane enzyme that belongs to the group of hydrolases. It is necessary in order that the body was carried out the reaction of dephosphorylation, namely, the cleavage of phosphate from organic substances. The name of the alkaline enzyme was for the fact that most activity he has shown in the pH range from 8.6 to 10.1. A family of isoenzymes of alkaline phosphatase consists of TNSF encoded in the gene ALPL, as well as placental, embryonic, and intestinal alkaline phosphatase, encoded by the genes ALPP, ALPP2 and ALPI, respectively. TNSF only isoenzyme involved in the mineralization of tissues 1.
Mineralization of cartilage, bones and teeth – a process occurring in several stages, the result of which is the deposition of hydroxyapatite in the extracellular space. Hypertrophic chondrocytes, osteoblasts and odontoblast contain matrix vesicles (vesicles) that are embedded in the membrane, rich annexins A2, A5, A6, CA-ATPase, alkaline phosphatase, nucleotide phosphate-phosphoesterase (NPP), cotransporters Pit 1 and PHOSPHO 1 1. PHOSPHO 1 is magnetovolume the hydrolase, which is expressed in mineralized tissues. NPP is a group of enzymes capable to hydrolyze diesters and phosphoric acid in phosphomonoesterase. These enzymes are involved in many body processes, including mineralization, are the suppliers of intracellular and extracellular inorganic phosphate (Pi).
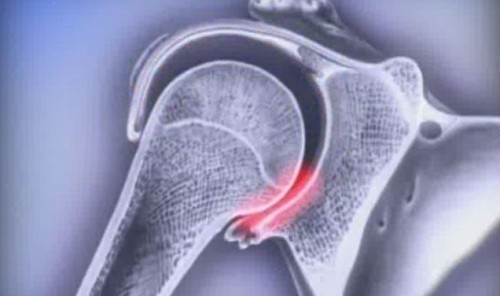
The first stage of mineralization takes place within matrix vesicles, which are formed crystals of hydroxyapatite. Hydroxyapatite is the main inorganic component of bone tissue. Membrane phospholipids are hydrolyzed by phospholipase C to phosphocholine and phosphoethanolamine. Then these compounds are hydrolyzed PHOSPHO 1 to obtaining inorganic phosphate. Another source of inorganic phosphate in matrix vesicles is a Pit 1 – Na/Pi cotransporter. Calcium enters the vesicle through the annexin-CA-channel (Fig.).

The resulting crystals of hydroxyapatite pinetreeroad matrix vesicles and penetrate into the extracellular space where, ultimately, are deposited between the collagen fibrils to complete mineralization within the extracellular matrix. The ratio of inorganic phosphate to inorganic pyrophosphate (PPi) is crucial in the second stage of mineralization. Inorganic pyrophosphate is an inhibitor of the formation of hydroxyapatite. Inorganic pyrophosphate is formed in two ways: in the extracellular space of ATP by membrane enzyme NPP1and also penetrates from the cytoplasm, where it is formed during cellular metabolism through the transport of transmembrane surface protein ANKН, the human homologue of the mouse progressive ankylosis protein (ANK) – cotransporter, which is present on the membrane of chondrocytes and osteoblasts. TNSF also located on the membrane of matrix vesicles and the hydrolysis of inorganic pyrophosphate to inorganic phosphate, thus promoting the formation of hydroxyapatite.
In mice the lack of NPP1 or ANK lead to calcification of soft tissues, including blood vessels, by reducing the level of PPi. In contrast, mice with deficiency TNMF showed the clinical picture the infant form of GF. At 6-10 days after birth showed signs of hypomineralization, on the 20th day the mouse died. Violation of mineralization occurred as a result of violation of synthesis of hydroxyapatite due to the high concentration of PPi.
Hypophosphatasia develops as a result of a defect function TNDF that leads to impaired mineralization. Alkaline phosphatase deficiency leads to suppression of the synthesis of hydroxyapatite in the extracellular space. However, matrix vesicles mineralization is normal. Thus, in patients with GF bone matrix remains demineralizovannaja, which leads to rickets and osteomalacia.
Another role of alkaline phosphatase is the Association with the synthesis of neurotransmitters in the Central nervous system (CNS). Pyridoxal 5′-phosphate (PLP) is the main circulating form of vitamin B6 is a coenzyme of glutamic acid decarboxylase, which is responsible for the synthesis of GABA. With the help of AP is the dephosphorylation of PLP, resulting in the formation of pyridoxal, which can cross the blood-brain barrier, and then to recover in PLP. Alkaline phosphatase deficiency leads to the lack of PLP in the CNS, which is clinically manifested vitamin B6-dependent seizures 1.
Clinical forms hypophosphatasia and their manifestations
Hypophosphatasia the clinical picture varies with age.
1. Perinatal (severe, lethal) form. Can be diagnosed in utero or immediately at birth. Is characterized by a complete lack of bone mineralization of the skeleton, osteochondral spurs, protruding through the skin of the forearms and legs (the pathogenesis of these manifestations is unknown), the substantial shortening of the long bones, convulsive disorder 12. Without replacement therapy children die within a year 3. All the newborn required ventilation support because of severe respiratory failure due to pulmonary hypoplasia and biomechanical disorders of the act of breathing due to rachitic changes in the chest.
2. Infant (benign, infantile) form. Manifested respiratory failure and vitamin b6–dependent seizures in the first 6 months of life, and pronounced muscular hypotonia. Because suppressed the formation of hydroxyapatite decreases the uptake of calcium by bone, which leads to hypercalcemia, hypercalciuria and, as a consequence, to nefrocalzinoz. In addition, often there is craniosynostosis, which is a dangerous increase in intracranial pressure and development of edema of the optic nerve, which requires a craniotomy. It remains unclear pathogenesis of the occurrence of craniosynostosis 15. Without replacement therapy the mortality is 50% to 9 months of life 16.
3. Juvenile form. Typical symptoms are early (up to age 5 years) loss of teeth, bone pain, bone deformities characteristic of rickets (funnel chest, deformity of limbs, rachitic rosary), frequent, poorly healing fractures. Children can have significant delay of motor development. In some cases, wrongly diagnosed with chronic recurrent multifocal osteomyelitis, which is characterized by lose metafit long bones, bone marrow edema, periarticular pain, soft tissue swelling 25. Slow bone growth due to the violation enchondral ossification as in rickets. Softening of bone tissue as the result of defective mineralization of osteoid at sites of remodeling, as well as violations of salinity on the growth phases on the surface of the periosteal blood lead to the inability to increase the width of the bone, forming a narrow bone that is easily bent, which can lead to significant deformation. Chest adopts the funnel shape, the ribs are unable to adequately participate in a breath, arise atelectasis, worsening of gas exchange and, as a consequence, respiratory failure 13.
In General, the prognosis is relatively favorable. However, depending on the manifestations of the disease, quality of life can suffer.
4. Adult form. Typical symptoms are osteoporosis, recurrent low-energy fractures and pain in bones and muscles, headaches, dental anomalies. Fractures are usually localized in the radial, humeral bones; in women, common intertrochanteric fractures of the femur, fractures of the metatarsal bones, in men, vertebral fractures 17.
The disease may start also with a crystal arthropathy. The deposition of calcium pyrophosphate in the ligaments, tendons and joints may be cause of pain and limitation of motor activity 4.
S. S. Rodionova et al. 11 described two cases of CSF in adults. In one case the GF was detected in women with the clinical and radiological picture similar to postmenopausal osteoporosis, complicated by a compression fracture of a vertebra, wherein only a reduced level of alkaline phosphatase. In another case in a patient with aseptic necrosis of the femoral head detected a low level of alkaline phosphatase in the genetic study confirmed the diagnosis of GF and recommended treatment astazou alpha* in the postoperative period.
5. Odontohypophosphatasia. Characterized by problems with teeth and eliminates any skeletal manifestations. On the condition of the teeth affects both the absence of cement, and the violation of the formation of the enamel, leading to tooth decay.
The alkaline phosphatase level may be slightly below normal or within the normal range, therefore, in any patient with unexplained premature loss of the milk and/or permanent teeth should be suspected odontohypophosphatasia. In addition to premature loss of teeth, odontohypophosphatasia is characterized by the reduced height of the alveolar bone, the root of the abnormally short and extended polyarnoi camera. In addition, the frequently observed hypoplasia of the enamel, dentin dysplasia and hypoplasia of the cement. Gingivitis and periodontitis are rare 23.
Diagnosis
Hypophosphatasia diagnosis is difficult because the disease is rare and symptoms are primarily identifitseerida as more common diseases. Diagnostic criteria the global Fund has not developed. The main feature of GF is the low level of alkaline phosphatase of blood serum.
Laboratory diagnosis
1. Alkaline phosphatase blood reduced.
It should be remembered that the reference values of alkaline phosphatase vary with age and gender and may vary slightly depending on the laboratory. Alkaline phosphatase may be elevated during pregnancy. A slight increase can be observed also in diseases of the liver, and fresh fractures in the postoperative period. For these reasons, it is necessary several times to repeat the analysis if you suspect a GF.
Quantitative analysis of bone alkaline phosphatase is usually not required. However, liver diseases, pregnancy, in postoperative period, total alkaline phosphatase can be lognormal 3.
2. The concentration of phosphoethanolamine (pea) in urine is increased.
Phosphoethanolamine along with pyridoxal-5-phosphate and inorganic pyrophosphate is a substrate for alkaline phosphatase, which accumulates in plasma and urine at deficiency of alkaline phosphatase. This is the second analysis that you must perform if you suspect a GF. Elevated levels of pea speaks in favor of the diagnosis of GF. However, this figure may increase when other metabolic diseases, or sometimes to have a normal level in patients with TGF 3, 11. Asymptomatic heterozygous carriers of the mutation may have increased the concentration of FEA 3.
3. The concentration of pyridoxal-5-phosphate in the blood is increased.
Due to the shortage of alkaline phosphatase occurs dephosphorylation of PLP, pyridoxal, therefore, does not penetrate the blood-brain barrier, and PLP accumulates in the systemic circulation.
Biologically active metabolite of vitamin b6 may be the most sensitive indicator of GF. During the week before the test is not recommended to use vitamin supplements to avoid the false positive result 3.
As a rule, the heavier form of GF in children, the lower the concentration of alkaline phosphatase and higher concentration of pyridoxal-5-phosphate in the plasma 8. Pyridoxal-5-phosphate is likely correlated with the occurrence of fractures and the number of symptoms in adults 5.
4. The concentration of total calcium, ionized calcium, inorganic phosphate in blood is normal.
Normal levels of these indicators distinguishes the global Fund from other forms of rickets. Hypercalciuria is without increasing the concentration of calcium in the blood. Although the concentration of phosphorus in the blood and urine in most cases remains within the reference values, it may be increased 3.
5. The concentration of vitamin D and parathyroid hormone in the blood is normal.
6. Inorganic phosphate in the urine was increased.
It is a sensitive marker of GF, which can also be elevated in asymptomatic carriers 3.
Treatment
When the diagnosis of GF requires a multidisciplinary approach to the treatment of the patient and prevention of complications.
Newborns may require artificial lung ventilation (ALV) or other methods of respiratory support. For children in the first year of life requires the supervision of a neurologist (prevention of seizures, the introduction of vitamin b6), a neurosurgeon (in the presence of craniosynostosis, surgical treatment), orthopedic (prevention and treatment of deformities of the skeleton), physical therapist (optimization of motor activity), the dentist. With hypercalcemia cope with the introduction of loop diuretics, restriction of calcium in the diet and limiting the amount of fluid intake.
Bone marrow transplantation is 8-month-old girl showed a significant clinical and radiological improvement. 7 years later the patient is active, has a clinical phenotype is a benign juvenile form of GF. In another case, bone marrow transplantation showed improvement functions, however caused drug leukemia 9. Transplantation of allogeneic mesenchymal stem cells of the donor, the isolated transplantation of osteoblasts also did not give sufficient effect 13.
In 1956, for the treatment of GF with limited success applied the cortisone. The use of replacement transfusion of plasma rich in alkaline phosphatase in patients with Paget’s disease was undertaken in the 1980-ies 13. These methods of treatment of GF also not successful.
In 2015, were tested pathogenetic therapy of recombinant human TGF tkanespecificescoe chimeric glycoprotein alkaline phosphatase – alpha astazou. This drug was used to treat patients with perinatal, infantile and juvenile forms of GF. Recommended p/to the injections 6 times a week 1 mg/kg body weight or 3 times a week for 2 mg/kg of body weight. The maximum injection volume of 1 ml 10. After 6-12 months of treatment was observed a positive dynamics in growth, motor development, respiratory function in 37 patients, however, still unknown to the delayed effect of treatment 24.
In a clinical study in Japan involved 13 patients, including 34-year-old man with a history of fracture of the humerus and left clavicle, gait disturbance, arthralgia. Reactions at the injection site was the most frequent adverse events. Serious adverse reactions, possibly related to the treatment astazou alpha, had seizures and hypocalcemia in a patient with perinatal form of GF. Recombinant enzyme stimulates mineralization in the bones, and this process requires the transport of calcium into the bone tissue, which may be the cause of hypocalcemia during treatment 22.
Asfaltata alpha registered today only for the treatment of pediatric forms of the GF, so data on the treatment of astazou alpha adult small. N. Ramde et al. 20 were treated with astazou alpha 59-year-old woman on hemodialysis with GF, which debuted in childhood. After 13 months of therapy with alpha asputisol the patient was an increase in mobility, decrease in pain, significant improvement of bone mineralization throughout the skeleton, including the consolidation of existing fractures and the absence of new fractures. This case shows the therapeutic success of treatment with alpha astazou adult patient with GF.
P. M. Camacho et al. 2 presented a report on the treatment of two women with GF teriparatide a dose of 20 mg subcutaneously daily for two years, and also describes 6 patients treated with teriparatide. All 8 patients were women 50 to 80 years. 3-6 months of treatment in patients increased levels of alkaline phosphatase and markers of bone resorption. Also described effects such as the reduction of pain in the bones, normalization of biochemical parameters during treatment, improvement in radiographic parameters 2. However, to confirm the positive influence of teriparatide in GF requires histological examination of bone that has not been submitted. Also described a case of successful treatment with teriparatide men with GF and end-stage chronic kidney disease 21.
According to other authors, teriparatide causes osteosarcoma in rats and may increase the risk of osteosarcoma in children (tumor growth), therefore, for the treatment of childhood forms GF the drug is not used 3.
Bisphosphonates (BP) is contraindicated in GF, since the mechanism of action is based on their structural analogy with pyrophosphates. Bisphosphonate group mimics pyrophosphate’s structure, thereby inhibiting activation of enzymes that utilize pyrophosphates. However, many patients remain undiagnosed GF, and they get treated BF.
In women suffering from the global Fund, described cases of atypical intertrochanteric fractures of the femur, which occur also with long-term therapy of BF and associated with a slowdown of bone metabolism 18, 19. Probably, the reception BF in a patient with CSF may exacerbate the slow exchange bone tissue that may lead to atypical fractures of the thigh. Data on the frequency of complications of such treatment at the moment. Described the case of a sharp decline in bone mineral density and occurrence of multiple fractures in men after starting alendronate. In the same period, the patient developed chronic kidney disease, and also identified TGF. It is difficult to say which factor was affected by the violation of bone metabolism 26.
It should also be avoid additional intake of vitamin D, except in cases of obvious deficiency, because traditional treatment of rickets and osteomalacia methods can increase the hypercalciuria and hypercalcemia, which is often observed in severe forms of GF. However, there is no need to limit sun exposure and consumption of foods rich in vitamin D as there is a risk of rickets caused by vitamin D deficiency as a concomitant disease in the GF 3.
Conclusion
Hypophosphatasia is a rare and poorly understood disease. However, correct diagnosis is very important, since the adult form of GF is often erroneously interpreted as osteoporosis. Correct diagnosis can prevent unnecessary use of bisphosphonates and choose the more adequate treatment.
Clinical manifestations of CSF in adults is extremely varied: as a rule, in patients with the adult form of the GF in the anamnesis there is an instruction on the manifestations of rickets in childhood or early loss of teeth (milk or permanent) can take place complaints of musculoskeletal pain, frequent, poorly fused fractures, fatigue, gait changes, nephrocalcinosis.
The question remains of GF prevalence among the adult population, as well as the frequency of occurrence of various clinical symptoms. According to some, women are less likely to suffer from fractures, while among men it was noted the rare development of dental problems, complaints of muscle pain and headaches 5.
Not diagnostic criteria in GF. In addition, at the moment, there are no treatment guidelines for CSF in adults. Clinical studies afatasi Alfa in adults was conducted.
Considering the above problems, it is required to study this disease further development of clinical guidelines for the management of patients with the adult form of GF.
Literature
- Orimo H. Pathophysiology of hypophosphatasia and the potential role of asfotase alfa // Therapeutics and Clinical Risk Management. 2016; 12: 777-786.
- Camacho P. M., Mazhari M. A., Wilczynski, C., Kadanoff R., Mumm, S., Whyte M. P. Аdult hypophosphatasia treated with teriparatide: report of 2 patients and review of the literature // Endocr Pract. 2016; 22 (8): 941-950.
- Mornet E., Nunes M. E. Hypophosphatasia. In: R. A. Pagon, M. P. Adam, H. H. Ardinger et al., eds. University of Washington, GeneReviews (R). Seattle, WA, 1993.
- .. Guanabens N., Mumm S., Möller I. Calcific Periarthritis as the Only Clinical Manifestation of Hypophosphatasia in Middle Aged Sisters // J Bone Miner Res. 2014; 29 (4): 929-934.
- Schmidt T., Mussawy N., Rolvien T., Hawellek T., Hubert J., Rüther W, Amling M., Barvencik F. Clinical, radiographic and biochemical characteristicsof adult hypophosphatasia // Osteoporosis International. 2017, 28 (9): 2653-2662.
- Tadokoro M., Machida H., Ohgushi H. Genetic basis for skeletal disease. Stem cell therapy for genetic bone disorders // Clin Calcium. 2010; 20 (8): 1228-1235.
- Whyte M. P., Zhang F., Wenkert, D., McAlister W. H., Mack, K. E., Benigno, M. C., Coburn S. P., S. Wagy, Griffin D. M., Ericson, K. L., Mumm S. Hypophosphatasia: validation and expansion of the clinical nosology for children from 25 years experience with 173 pediatric patients // Bone. 2015, 75: 229-239.
- Whyte M. P., Walkenhorst, D. A., Fedde K. N., Henthorn PS, Hill C. S. Hypophosphatasia: levels of bone alkaline phosphatase immunoreactivity in serum reflect disease severity // J Clin Endocrinol Metab. 1996, 81 (6): 2142-2148.
- Taketani T., Kanai R., Abe M., Mishima S., Tadokoro, M., Katsube Y., Yuba, S., Ogushi, H., Fukuda S., Yamaguchi S. Therapy-related Ph+ leukemia after both bone marrow and mesenchymal stem cell transplantation for hypophosphatasia // Pediatr Int. 2013; 55: 52-55.
- STRENSIQTM (asfotase alfa) for Strensiq prescribing information. Cheshire, CT: Alexion Pharmaceuticals, Inc; 2015. Available from: http://strensiq.com/images/pi.pdf. Accessed March 18, 2018.
- Rodionova S. S., Zakharova E. Yu., despite the presence of U. V., Khakimov R. W., S. V. Lapkina Hypophosphatasia in adults: clinical cases and review of the literature // Osteoporosis and osteopathy. 2015, № 2. Pp. 25-27.
- Kulikova K. S. Kalinchenko N. Yu, Sibileva E. N., Vasilyev E. V., Petrov V. M., Tulpakov A. N. Hypophosphatasia: clinical description of three cases with molecular genetic diagnosis verification // Problems of endocrinology. 2015, № 3. Pp. 37-42.
- Bishop N. Clinical management of hypophosphatasia // Clinical Cases in Mineral and Bone Metabolism. 2015; 12 (2): 170-173.
- Mornet E., A. Yvard, A. Taillandier, D. Fauvert, Simon-Bouy B. Amolecular-based estimation of the prevalence of hypophosphatasia in the European population // Ann Hum Genet. 2011; 75 (3): 439-45.
- Mornet E., Whyte, M. P. Alkaline Phosphatase and Hypophosphatasia // Calcif Tissue Int. In 2016; 98: 398-416.
- Leung, E. C., Mhanni, A. A., Reed M., Whyte M. P., Landy, H., Greenberg C. R. Outcome of perinatal hypophosphatasia in manitoba mennonites: a retrospective cohort analysis // JIMD Rep. 2013; 11: 73-78.
- Berkseth, K. E., Tebben, P. J., Drake M. T. Clinical spectrum of hypophosphatasia diagnosed in adults // Bone. 2013; 54 (1): 21-27.
- Whyte M. P. Atypical femoral fractures, bisphosphonates, and adult hypophosphatasia // J Bone Miner Res. 2009; 24 (6): 1132-1134.
- Lawrence J. E., Saeed D., Bartlett J., Carrothers, A. D. Adult-onset hypophosphatasia diagnosed following bilateral atypical femoral fractures in a 55-year-old woman // Clin Cases Miner Bone Metab. 2017; 14 (3): 347-353.
- Cooper M. S., M. Quinkler, H. Remde Successful Asfotase Alfa Treatment in an Adult Dialysis Patient With Childhood-Onset Hypophosphatasia // J Endocr Soc. 2017; 1 (9): 1188-1193.
- Cundy T., T. Michigami, and K. Tachikawa, M. Dray, J. F. Collins, E. P. Paschalis, S. Gamsjaeger, A. Roschger, Fratzl-Zelman N., Roschger P., Klaushofer K. Reversible deterioration in hypophosphatasia caused by renal failure with bisphosphonate treatment // J Bone Miner Res. 2015; 30 (9): 1726-1737.
- Kitaoka T., Tajima T., Nagasaki K., Kikuchi, T., Yamamoto, K., Michigami, T., Okada S., Fujiwara I., Kokaji M., Mochizuki H., Ogata T., Tatebayashi, K., Watanabe A., Yatsuga S., Kubota T., Ozono K. Safety and efficacy of treatment with asfotase alfa in patients with hypophosphatasia: Results from a Japanese clinical trial // Clin Endocrinol (Oxf). 2017; 87 (1): 10-19.
- Wang Z. Y., Zhang K., Zheng G. S., Qiao, W., Su X. Y. Current concepts in odontohypophosphatasia form of hypophosphatasia and report of two cases // BMC Oral Health. 2016; 16 (1): 1-8.
- Whyte M. P., Rockman-Greenberg C., Ozono K. Asfotase alfa treatment improves survival for perinatal and infantile hypophosphatasia // Journal of Clinical Endocrinology and Metabolism. 2016; 101: 334-342.
- M. P. Whyte, D. Wenkert, W. H. McAlister, M. Z. Mughal, Freemont A. J., Whitehouse R. Chronic recurrent multifocal osteomyelitis mimicked in childhood hypophosphatasia // J Bone Miner Res. 2009; 24 (8): 1493-1505.



You are a very capable person!