Dental implants today is the best way of replacing missing teeth. More and more people prefer implants instead of traditional removable dentures or prosthetic teeth.
This is primarily due to the high functional stability of implants and the possibility to achieve an aesthetic result. Competition in the market of dental products leads to the fact that every year, the implantation becomes more accessible to people.
However, in addition to the indisputable advantages of implantation, there are a number of contraindications to this type of treatment. It severely limits the number of potential patients. Moreover, there are other factors that force people to abandon this type of restoration of the dentition.
First and foremost is the financial difficulties faced by the people when he finds out the cost of complex treatment. The second reason is the fear of the patient’s potential rejection of the implant. As a rule, the question of financial possibilities is the most frequent cause of failure of the implant.
The fear of rejection is usually seen in a small number of people, often those who had bad experiences with implantation. Nevertheless, the question of rejection of implants are now actively being explored by leading manufacturers of dental equipment. Constantly improved production technology, processing and coating of implants, which improves the statistics of successful osseointegration. However, the individual characteristics of each organism always create some risk on the way to achieving the desired result.
Why the implant is rejected?
There are many reasons that can lead to loss of the implant. In each case unsuccessful implantation has its own unique set of factors that together led to unsatisfactory results. However, if each situation to identify the main reason, the most popular will be: peri-implantitis and mucositis, proper implant failure, allergic reaction, complications related to maxillary sinus, failure of the implant.

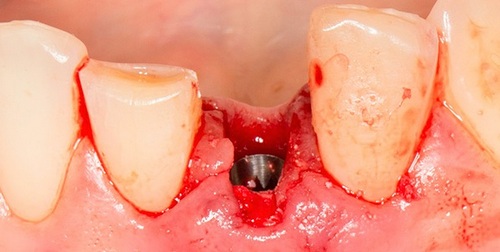
Peri-implantitis
Periimplant is an infectious inflammatory destructive disease that affects the bone structure and soft tissue around the implant. It is worth noting that among the reasons for unsuccessful implantation this complication takes a leading role. Hence, this complication and afraid patients, which often leads to refusal to perform dental implantation. A trigger in the development of this disease can serve a multitude of factors.
Low-quality implants can be made of cheaper alloys have a coating that is not conducive to engraftment of the implant. Also, the cause may be improper operation. Errors can be in violation of the rules of asepsis and antisepsis, the deviation from the protocols of the bone (bone overheating, the wrong choice of cutters, etc.), fixation of orthopedic structures.
Also pay attention to the hygiene after the implantation. Many people of middle and Mature age, are unable to adapt to a new, more durable method of care for the oral cavity. This leads to the appearance of caries on the remaining teeth and the development of inflammatory diseases, such as mucositis, gingivitis, periodontitis.
Cause of snoring can also be the installation of implants to the patient whom they are contraindicated. Many people prefer not to tell the dentist about their somatic diseases. This happens for various reasons. Some patients do not consider this information necessary to perform the operation in the oral cavity. Others fear that the doctor will refuse to treat with implants, and then have to use removable prosthesis. In the end, there is a complication that can lead to loss of the implant.
The clinical picture of peri-implantitis resembles the aggravation of periodontitis. In the affected area of the mucous membrane acquires a bright red hue. When brushing teeth the gums surrounding the implant may need to bleed. Often a symptom of peri-implantitis is a fistula, which appears on the gums in the projection of the implant. The General condition is disturbed, however, not always it is possible to increase body temperature and symptoms of intoxication. The mobility of the implant is observed in the case that peri-implantitis occurred in a short time after the screwing of the implant or advanced stages of the disease.
For the diagnosis of periimplantitis is necessary to analyze the radiographs. Depending on the extent of bone destruction around the implant is determined by the extent of the disease. The first class of peri-implantitis appears in the form of a slight horizontal bone destruction of tissue. The second class is characterized by moderate horizontal loss of bone tissue and the formation of a unilateral vertical bone defect in the region of the implant. The third class differs from the second by the fact that the vertical defect surrounding the implant on all sides. At this stage you may experience the mobility of the implant. The fourth stage is characterized by a pronounced degree of resorption of bone with the destruction of one of the walls of the alveolar process.
Treatment of snoring should begin as early as possible. Only under this condition it is possible to save the implant and to avoid the negative consequences (removal of implant). Methods of elimination of inflammatory-destructive process in the first place depends on the stage of the pathological process. Moreover, the importance is at what stage implantation occurred peri-implantitis. If the implant is at the stage of osseointegration, perform incision, create access to the implant and twisting of his cap. After that, the wound washed with antiseptic solutions and set the healing abutment.
After the appointment of a medical anti-inflammatory treatment, symptoms disappear in 3-4 days. A week after the therapy, the healing abutment is removed and screwed the plug. If performed correctly, manipulation of the wound is self-locked. The second and third stages require additional manipulations, which consist in the introduction of bone substance in the area of resorption. Fourth grade peri-implantitis can be treated by the same procedure, but the chances of success are minimal. Often requires removing the implant by reimplantation after 6 months.
Mucositis and hyperplasia of the mucous membrane
Mucositis is a less dangerous complication than peri-implantitis. It is connected primarily with the fact that the pathological process affects only soft tissue around the implant. If we draw a parallel with the classic dental disease, mucositis can be compared with gingivitis and periimplantitis – periodontitis. However, despite the relative insignificance of mucositis, it should be treated seriously because it can be complicated by peri-implantitis. The most common cause of this disease is acute trauma any infection on the wound surface, chronic injury and violation of the rules of care for the oral cavity.
Mucositis the clinical picture is manifested by redness, cyanosis, and swelling in the affected area. People may complain of pain, itching, burning, viscosity of saliva, disomfort mouth. Around the implant sometimes is determined by the growth of granulations, which suggests the existence of processes of hyperplasia. On the x-ray image changes are not detected.
Treatment of mucositis is to remove its causes. For this, the doctor performs a professional dental cleaning, appoints antiseptic and anti-inflammatory medications, and correct brushing technique. In the presence of granulation tissue in the area of the implant is performed a thorough curettage with an overlay of periodontal dressings.
Advancement of the implant into maxillary sinus
The penetration of the implant into the maxillary sinus is quite rare, but this complication gives a person a lot of significant problems. The reason for the location of the implant in the maxillary sinus is primarily the incorrect treatment planning. Some of these clinics are trying to reduce the price for their services, refuse to observe the essential principles of implantology. For example, proper planning of treatment involves performing a CT scan, a thorough analysis and digital simulation of implantation.
The last point enables millimeter precision to determine the location of the future implant and its required size, diameter and shape. Thanks to the computer tomogram it is possible to see the boundaries of the maxillary sinus, to consider performing a sinus lift. If these stages are missed, the implant is unpredictable. For example, incorrectly chosen length of the implant may cause perforation of the maxillary sinus. As a result, the implant can completely fall into the sinus. Also factor in the risk of this complication is significant atrophy of the jaw. In this case, the area of the implant is too small, and the artificial bone after sinus lifting for a long time is in a soft condition. As a result, the implant can delve into the maxillary sinus.
The clinical picture of the progress of the implant in the maxillary sinus is quite unpredictable. For example, a foreign object caught in the maxillary sinus, can cause this inflammation (sinusitis). There are also cases where the implant exits through the nasal passages by sneezing. This suggests that in contact with the implant in the maxillary sinus is quite difficult to predict the outcome.
Treatment of this complication is to perform surgical intervention and removal of foreign object. The operation involves the creation of access through a lateral wall of the maxillary sinus with perforation fragment. After removal of the implant to the cut portion of the wall is laid in place and sutured. Re-implantation and tactics of its implementation is determined after establishing the cause complications and the condition of the maxillary sinus.
Allergic reaction
Titanium in modern medicine is one of the key metals. It is the best material for the manufacture of artificial joints, locking devices and dental implants. To date, Titan believes bioinert material, that is, it is biologically neutral to the tissues. It is this property allows the implant to integrate successfully into the bone substance. However, its biological properties is not fully understood. Some researchers argue that titanium can cause allergic reaction. But most experts do not share this opinion. They believe that the implant can cause allergies, but this fault is not titanium, and the impurities of other substances.
The fact that technologically very difficult to produce pure titanium. If large companies can afford it, the producers use cheap implants are not pure titanium. As a rule, the composition of the alloy includes actually titanium, iron, Nickel, silicon, carbon, and other elements. Their proportion in the alloy can vary depending on the technological and economic opportunities of the manufacturer. However, if we talk about allergies, it would be logical to assume that the impurities cause a reaction to the implant. It is argued that these substances do possess allergenic properties. But this theory is also at the research stage, so a specific answer, scientists still can not give.
The clinical picture of Allergy to the implant can be called a classic. Person concerned about dry mouth, burning, itching gums. For the diagnosis should conduct an Allergy test which will accurately identify the allergen and eliminate it.
The Allergy treatment should be based on individual clinical picture. Of course, the ideal method is to replace the implant for zirconium. However, not every patient is ready to start treatment all over again. Therefore, the first step is to conduct anti-allergic therapy. Only after that, in the absence of improvements, the design will have to be removed and replaced by zirconium. But, if improvements come, some time, you should carefully observe the condition of the implant.
Breakage of the implant
Most implants are made of very durable material – titanium. However, as mentioned earlier, many manufacturers save on research and technological stages. This allows them to compete with larger companies and offer consumers cheaper products. As a result, the market gets a lot of implant systems of rather low quality, which leads to unexpected complications after dental rehabilitation.
Dental implant fracture is a rare and dangerous complication. Besides being reduced to zero, the entire result of the treatment, and the doctor man get in serious trouble. First, the broken implant becomes movable. Therefore, the gap of the fracture can reach pathogenic microorganisms and cause inflammatory disease. It should also be noted that fragments of the implant needs to be removed completely. Can you get fused with the bone the implant is not an easy task even for an experienced surgeon.
If the implant was broken as a result of severe trauma, the task is complicated by the fact that together with the design lost a large number of human bone tissue.
The symptoms of implant failure
Implant failure is a disease which is accompanied by an inflammatory process in the bone around the implant. The difference of this process from periimplantitis is that when periimplantitis bone undergoes resorption only, and in this case it is a hotbed vospalitelnoe process. In fact, rejection of the implant can be called a local osteomyelitis.
The clinical picture of implant failure can manifest in several ways. On the boundary bone and implant possible the appearance of granulation tissue. The reasons for its formation can often be overheating the bone during preparation of the implant bed. Also a triggering factor may be non-sterile surface of the implant, which contains pathogenic microorganisms. In addition, do not forget about immune and hormonal system of the body which ensures the process of engraftment of the implant. If the systems works correctly, the integration of the implant is initially impossible.
The symptoms of implant failure are the following: pain, swelling and redness of the gums in the area of the implant. If the operation was carried out by one-stage method (when the intraosseous part and the abutment are one), then the person may feel the mobility of the structure. Moreover, the rejection of dental implant is often recovered by the patient in mind of too much movement. If dental rehabilitation was carried out on a two-stage procedure, the intraosseous part of the pressure independently of granulation tissue is pushed out. After that the inflammatory process is significantly reduced. On the radiograph is determined by the area of bone destruction around the perimeter of the implant width of about 1 mm. the Treatment of this condition involves removing the implant and conduct anti-inflammatory therapy. Re-implantation can be carried out not earlier than 6 months.
The second type of the clinical picture of rejection of the implant is characterized by the formation of sequestration, which contains the implant and the surrounding bone. Usually, this pathological process is triggered by significant overheating of the bone during its preparation, or the implantation in the area with low blood supply to bone tissue. A few days after the operation the person feels a dull pain in the region of implantation. Painkillers are only temporary, and anti-inflammatory medications do not produce the desired effect. In the first 14 days on the radiograph are not defined pathological processes, however, during this time, the implant may become mobile. The treatment of this form of rejection of the implant is to extract the implant, the relief of the inflammatory process and eliminate the resulting bone defect.
Preventing complications after implantation
Prevention of complications should be considered at the planning stage of treatment. Careful diagnosis, weighing the indications and contraindications, human motivation, his profession – all this has implications for predicting the outcome. Also you should always listen carefully and follow the instructions of the doctor. Even if you know how to perform hygienic procedures, re-obtaining this information will improve the result. After performing the implantation must not forget that the probability of occurrence of periimplantitis and implant failure always exists. And their triggering factor may be somatic pathology. Therefore, you should get rid of bad habits and practice a healthy lifestyle. This will prevent a lot of nasty diseases that are associated with all body systems. In sports you should always use protective devices. The observance of safety rules will prolong the life of implants for many years.
Whether to place implants?
Implantation is a complicated and complex dental rehabilitation. It has both advantages and disadvantages. After reviewing the various complications of implantation may be a question: “And whether it is necessary to place implants?” The decision is up to you. However, if you have the financial ability to undergo implantation, you should definitely perform this step. The fact that dental implants are the pinnacle of dentistry today. It has many advantages and high performance. With the help of implants can replace one tooth or all teeth of the upper and lower jaw. Restoration on implants are aesthetically pleasing and natural. A beautiful smile gives a person so much confidence that a successful implantation will stimulate the person to communicate more with people. This will open new opportunities in work, family and friendship.
Do not forget that after implantation in humans is possible, the correction of defects of speech. If impaired were associated with the absence of teeth or their improper location, the implant will allow the person to talk more serious and impressive.
Normal masticatory function is one of the most important factors in the health of the gastrointestinal tract. In the absence of teeth grinding food takes place substandard. As a result, the digestive process is less productive. Restoration on implants are characterised by a perfect anatomical shape, which allows high efficiency to chew food.
Durability
The service life of the implant is tens of years. This is due to the high structural strength and uniform load distribution and the teeth. In prosthetics bridges on teeth optimal service life is 10-15 years. It is worth noting that this option is quite good, if to speak about the prosthetic teeth. However, many people at a young age set bridges. Therefore, if in 30 years people will perform prosthetics, it is likely that in 45 years he will be without the denture and the abutment teeth. If was implanted, with proper care will remain the implant and the abutment teeth. Moreover, the implant can stand a lifetime. Removal of the implant after five years and more often associated with the occurrence of General somatic pathology.
Financial benefit
At first glance it seems that implants are very expensive form of treatment. However, their life fully justify their cost. For example, classic full dentures, you need to redo every 5 years. That is, for 20 years need four times to pass the prosthesis. Added to that the cost of retaining a paste that will probably need to clamp the lower denture. In the end, for 20 years, the amount spent on dentures will not be less than the cost of implantation. And if to compare quality of life with removable dentures and implantation, the latter option is more preferable and rational.




Is it okay if I link your article on FB? It’s very timely 😀
This is relevant advice for my followers, so I’ll share this article and you will probably get a few extra readers. It’s better than anything else I’ve seen when it comes to this topic. Thanks for the fresh info!
This entry gives so much more info than other people, and it’s incredibly useful to me. Will be returning to read more writing from you! can I share this?
Enjoyed examining this, very good stuff, thanks .