At 32, Cara Hoofe was so constantly exhausted she could barely keep her eyes open, but assumed this was due to her hectic lifestyle. A woman’s aggressive bowel cancer was missed by doctors for a whole year because they thought she was too young to get it.
But when her condition worsened, and she began having stomach cramps and constipation, she sought advice from her GP. He sent her away with iron tablets for anaemia, despite her family history of bowel cancer – her father was diagnosed in his 40s.
Cara, now 34, was shocked to discover she had advanced cancer, which meant she had to have a large part of her bowel removed. It had also spread to her liver, and part of that had to be cut away too.
Just like her doctor, the merchandising worker never expected she would get the disease at her age – most people diagnosed are over 60.
But she found out she had Lynch syndrome (LS), an inherited condition which brings a higher risk of developing bowel, ovarian and womb cancer. It doesn’t cause any symptoms until the disease strikes.
At 32, Cara Hoofe was so constantly exhausted she could barely keep her eyes open, but assumed this was due to her hectic lifestyle

But when her condition worsened, and she began having stomach cramps and constipation, she sought advice from her GP (pictured in hospital after having surgery)
WHAT IS LYNCH SYNDROME?
Lynch syndrome (LS) is a condition that can run in families. It is also known as hereditary non-polyposis colorectal cancer (HNPCC). It is caused by an alteration in a gene called a mismatch repair gene. Carriers do not have any symptoms.
But people with the syndrome have an increased risk of developing bowel, womb and ovarian cancer. If your family has a history of developing these cancers when they are under 50 years old, it is possible they have the altered gene that causes LS.
Bowel cancer that doesn’t run in families usually develops in people over 50. But for people with LS, bowel cancer usually develops between the ages of 40 and 50 or younger. Being aware of your normal bowel habits is important, particularly if you have or think you may have LS.
Be aware of:
- Blood on or in your stools (poo).
- Diarrhoea, constipation or another change to your bowel habit that lasts longer than six weeks and has no obvious reason.
- Unexplained weight loss.
- Pain in the tummy or back passage.
- A feeling of not having emptied your bowel properly after you go to the toilet.
LS is the most common cause of hereditary bowel cancer. It means a carrier’s lifetime risk of bowel cancer is 50 to 80 per cent. Women with the condition have 30 to 60 per cent risk of womb cancer and a 10 per cent risk of ovarian cancer.
And despite undergoing grueling treatment, Cara has an 80 per cent chance of the disease returning at some point in the future. ‘It wasn’t really something I thought about – although the possibility started nagging me, when I began to feel ill,’ said Cara, from Maida Vale, west London.
She said: ‘I was shocked to be diagnosed so young.
‘I do think a lot of people thought I was too young for bowel cancer and that leads to delays in diagnosis.
‘My GP had never seen it in anyone as young as me before. It’s seen as an older person’s disease.’
Year-long search for answers
Shortly after her milestone birthday, Cara began feeling permanently exhausted and run down.
For months, she attributed it to her busy lifestyle taking its toll, now she was no longer in her twenties.
‘I’d been unusually tired for months but I just dismissed it as something that just happens when you turn 30,’ she said.
‘It makes me chuckle as if reaching 30 puts you on some slippery slope to the realms of being an OAP.

He sent her away with iron tablets for anaemia, despite her family history of bowel cancer – her father was diagnosed in his 40s (pictured with her mother Andrea)
‘I hadn’t dreaded it. It hadn’t really crossed my mind, but when I started feeling sick, I thought it’s probably because I am getting old.’
But in January 2015, she saw her GP after having stomach cramps and constipation.
‘I knew there was a slight genetic link with bowel cancer, so it was somewhere at the back of my mind now I felt ill,’ she said.
‘I mentioned to my GP that my dad had bowel cancer, but I didn’t have any of the major symptoms, like blood in my stools, so it wasn’t the first thing we investigated.’
Noticing she looked anaemic, her GP prescribed her iron tablets – the start of a 10-month journey, ruling out problems like fibroids, before her cancer was discovered.
Cara said: ‘Because I was so young, I think even the doctors thought it was unlikely I’d have bowel cancer.’
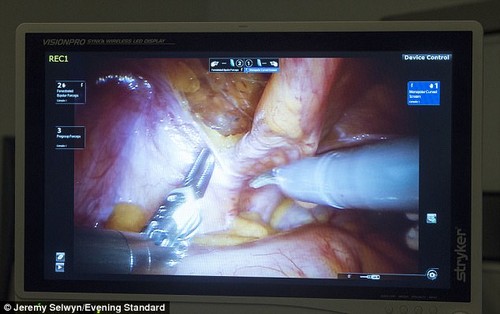
But, when the iron tablets failed to work, her GP had one of her stool samples tested – finding blood in it, not visible to the naked eye. Cara was shocked to discover she had advanced cancer, which meant she had to have a large part of her bowel removed. It spread to her liver, and part of that had to be cut away too
After that, she was referred to Imperial Hospital London for a colonoscopy, where a telescopic camera is used to examine the lining of the bowel for abnormalities. The same day the results revealed a tumour in the right side of her bowel. At that stage she didn’t know it was cancerous.
A week later she found out it was malignant. It was stage three, which means it hadn’t spread, and T4, which means it was locally advanced.
Cara said: ‘When I reached the point where the doctor actually told me I had cancer, in January 2016, I think I already knew, because it felt like I was following the same path as my dad did before his diagnosis.
‘I had started to prepare for that but it was still overwhelming when it happened.’
Cancer had spread
Around a month later, in February 2016, Cara began chemotherapy at Charing Cross Hospital in London. Then, when she was four cycles into the six-cycle course, on her GP’s advice, she was admitted to hospital, in extreme pain.
It is still unclear what was causing the pain – but doctors performed emergency surgery to remove a large section of her bowel. The tumour was removed at this point as well. Just like her doctor, the merchandising worker never expected she would get the disease at her age – most people diagnosed are over 60 (pictured: her scar after surgery)
After a three-month recovery period, Cara was given more chemotherapy to remove the last few traces of cancer. But, she was dealt more heartache when, as she neared the end of the treatment, further lesions were found on her liver – meaning she would need even more intensive chemotherapy.
Last month, she had four-hour surgery at Hammersmith Hospital to have part of her liver removed in a bid to prevent the cancer from spreading. Although she faces more chemo, she hopes to be discharged from the oncologist next year.
Eggs frozen
Because chemotherapy can damage fertility, Cara had her eggs frozen ahead of the treatment. However, she is re-thinking her plans to have children in the future, in case she passed on her faulty genes.
If someone with LS has children, they will have a 50 per cent risk of inheriting the altered gene.
She said: ‘I wasn’t in a place where I was thinking about children when I was diagnosed, but it was always my dream to have them one day.
‘Now, I’m not sure if I would want to go ahead with that and risk my children picking up a faulty gene and having cancer.
‘I know there are things that can be done to test if you have IVF, but it’s a lot to have to go through.
‘It’s all quite overwhelming, as I’m thinking about treatment at the same time.’
She found out she had Lynch syndrome (LS), an inherited condition which brings a higher risk of developing bowel, ovarian and womb cancer (pictured with her friend Susannah Brooke)
Now she is raising money for charity Shine Cancer Support by walking the length of the Thames. So far, she has completed around 70 miles, and will continue to walk the remaining 110 miles in stages.
She is also sharing her story to help raise awareness of Bowel Cancer UK’s Never Too Young Campaign, which aims to give younger bowel cancer patients a voice, change clinical practice and stop the disease in people under 50.
At the moment, the NHS offers bowel screening to over 55s, although a recent study, conducted by a French team led by Dr David Karsenti, has advised this should be lowered to 45.



I’d have to examine with you here. Which is not one thing I usually do! I take pleasure in reading a post that may make folks think. Additionally, thanks for permitting me to comment!
Oh my goodness! Impressive article dude! Many thanks, However I am having difficulties with your RSS. I don’t understand the reason why I am unable to subscribe to it. Is there anybody else having similar RSS problems? Anyone that knows the answer can you kindly respond? Thanx!!