The choice of treatment tactics for various forms of atrial fibrillation is aimed at restoring and maintaining sinus rhythm, preventing recurrent attacks of atrial fibrillation, monitoring heart rate, preventing thromboembolic complications.
For the relief of paroxysmal atrial fibrillation, the use of procainamide (intravenously and orally), quinidine (inside), amiodarone (intravenously and inside) and propafenone (inside) under the control of blood pressure and electrocardiogram is effective.
The use of digoxin, propranolol and verapamil gives a less pronounced result, which, however, by reducing the heart rate, contributes to the improvement of patients’ well-being (dyspnea, weakness, palpitations). In the absence of the expected positive effect of drug therapy, electric cardioversion (applying a pulsed electrical discharge to the heart area to restore the heart rhythm) is resorted to, relieving paroxysm of atrial fibrillation in 90% of cases.
When atrial fibrillation lasts for more than 48 hours, the risk of thrombus formation increases dramatically, so warfarin is prescribed to prevent thromboembolic complications. To prevent the recurrence of atrial fibrillation after restoration of sinus rhythm, antiarrhythmic drugs are prescribed: amiodarone, propafenone, etc.
When a chronic form of atrial fibrillation is established, a permanent intake of adrenergic blockers (atenolol, metoprolol, bisoprolol), digoxin, calcium antagonists (diltiazem, verapamil) and warfarin (under the control of coagulogram indices – prothrombin index or INR) is prescribed. In atrial fibrillation, treatment of the underlying disease that leads to the development of a rhythm disorder is necessary.
The method of radically eliminating atrial fibrillation is radiofrequency isolation of the pulmonary veins, during which the focus of ectopic excitation, located in the mouths of the pulmonary veins, is isolated from the atria. Radiofrequency isolation of the mouth of the pulmonary veins is an invasive technique, the effectiveness of which is about 60%.

With frequent attacks of atrial fibrillation or with its constant form, it is possible to perform RFA of the heart – radiofrequency ablation (“burning” with the help of an electrode) of the atrioventricular node with the creation of a complete transverse AV-blockade and implantation of a permanent pacemaker.
Atrial fibrillation (atrial fibrillation) is a heart rhythm disorder accompanied by frequent, chaotic agitation and contraction of the atria, or twitching, fibrillation of certain groups of atrial muscle fibers. Heart rate in atrial fibrillation reaches 350-600 per minute. With prolonged paroxysm of atrial fibrillation (greater than 48 hours), the risk of thrombosis and ischemic stroke increases. With a constant form of atrial fibrillation, a sharp progression of chronic circulatory failure can be observed.
Atrial fibrillation is one of the most common variants of arrhythmias and makes up to 30% of hospitalizations for arrhythmias. The prevalence of atrial fibrillation increases with age; it occurs in 1% of patients under 60 years old and in more than 6% of patients after 60 years.
Atrial fibrillation (atrial fibrillation) is a heart rhythm disorder accompanied by frequent, chaotic agitation and contraction of the atria, or twitching, fibrillation of certain groups of atrial muscle fibers. Heart rate in atrial fibrillation reaches 350-600 per minute. With prolonged paroxysm of atrial fibrillation (greater than 48 hours), the risk of thrombosis and ischemic stroke increases. With a constant form of atrial fibrillation, a sharp progression of chronic circulatory failure can be observed.
Prognosis for atrial fibrillation
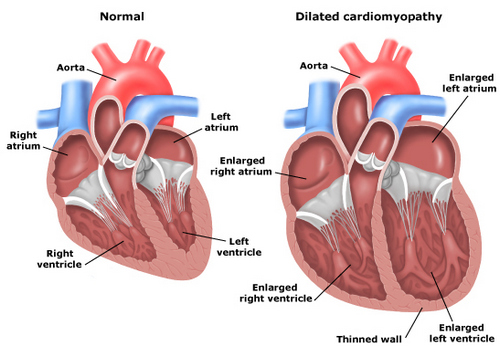
The main prognostic criteria for atrial fibrillation are the causes and complications of rhythm disturbances. Atrial fibrillation caused by heart defects, severe myocardial lesions (large-focal myocardial infarction, extensive or diffuse cardiosclerosis, dilated cardiomyopathy) quickly leads to the development of heart failure.
Thromboembolic complications due to atrial fibrillation are prognostically unfavorable. Atrial fibrillation increases mortality associated with heart disease, 1.7 times.
In the absence of severe cardiac disease and a satisfactory condition of the ventricular myocardium, the prognosis is more favorable, although the frequent occurrence of paroxysms of atrial fibrillation significantly reduces the quality of life of patients. When idiopathic atrial fibrillation state of health is usually not disturbed, people feel almost healthy and can do any work.
Classification of atrial fibrillation
The basis of the modern approach to the classification of atrial fibrillation includes the nature of the clinical course, etiological factors and electrophysiological mechanisms.
There are permanent (chronic), persistent and transient (paroxysmal) forms of atrial fibrillation. When paroxysmal form of the attack lasts no more than 7 days, usually less than 24 hours. Persistent and chronic atrial fibrillation last more than 7 days, the chronic form is determined by the ineffectiveness of electrical cardioversion. Paroxysmal and persistent forms of atrial fibrillation can be recurrent.
Distinguished for the first time an attack of atrial fibrillation and recurrent (second and subsequent episodes of atrial fibrillation). Atrial fibrillation can occur in two types of atrial arrhythmias: atrial fibrillation and atrial flutter.
During atrial fibrillation (atrial fibrillation), separate groups of muscle fibers are reduced, resulting in a lack of coordinated atrial contraction. A significant amount of electrical impulses are concentrated in the atrioventricular junction: some of them linger, others spread to the ventricular myocardium, causing them to contract with a different rhythm. In terms of the frequency of ventricular contractions, the tachysystolic (ventricular contractions of 90 or more per minute), normosystolic (ventricular contractions from 60 to 90 per minute), bradysystolic (ventricular contractions less than 60 per minute) of atrial fibrillation differ.
During the paroxysm of atrial fibrillation, no blood is pumped into the ventricles (atrial supplement). The atria contract inefficiently, so the diastole does not fill the ventricles with the blood that drains freely into them completely, as a result of which there is no periodic discharge of blood into the aorta system.
Atrial flutter is a rapid (up to 200-400 per minute) atrial contraction while maintaining the correct coordinated atrial rhythm. Myocardial contractions in atrial flutter follow each other almost without interruption, the diastolic pause is almost absent, the atria do not relax, being most of the time in systole. The filling of the atria with blood is difficult, and, consequently, the flow of blood into the ventricles decreases.
Every 2nd, 3rd or 4th impulse can flow through the atrio-ventricular connections to the ventricles, ensuring the correct ventricular rhythm – this is the correct atrial flutter. At disturbance of atrioventricular conductivity chaotic reduction of ventricles is noted, ie the wrong form of atrial flutter develops.
Causes of atrial fibrillation
Both cardiac pathology and diseases of other organs can lead to the development of atrial fibrillation. Most often, atrial fibrillation is associated with the course of myocardial infarction, cardiosclerosis, rheumatic heart disease, myocarditis, cardiomyopathy, arterial hypertension, and severe heart failure.
Sometimes atrial fibrillation occurs when thyrotoxicosis, intoxication with adrenomimetics, cardiac glycosides, alcohol, can be provoked by neuropsychic overloads, hypokalemia.
Also found idiopathic atrial fibrillation, the causes of which remain undetected even with the most thorough examination.
Symptoms of atrial fibrillation
Manifestations of atrial fibrillation depend on its form (bradysystolic or tachysystolic, paroxysmal or permanent), on the state of the myocardium, valve apparatus, individual characteristics of the patient’s psyche. The tachysystolic form of atrial fibrillation is much more difficult. At the same time, patients feel heart palpitations, shortness of breath, aggravated by physical exertion, pain and interruptions in the heart.
Usually, at first, atrial fibrillation is paroxysmal, the progression of paroxysms (their duration and frequency) are individual. In some patients, after 2-3 attacks of atrial fibrillation, a persistent or chronic form is established, in others, rare, short paroxysms are observed throughout life with no tendency to progression.
The occurrence of paroxysmal atrial fibrillation may be felt differently. Some patients may not notice it and find out about the presence of arrhythmia only during a medical examination. In typical cases, atrial fibrillation is felt by chaotic palpitations, sweating, weakness, trembling, fear, polyuria. With an excessively high heart rate, dizziness, fainting, Morgagni-Adams-Stokes seizures may occur. Symptoms of atrial fibrillation almost immediately disappear after the restoration of sinus heart rhythm. Patients suffering from persistent atrial fibrillation, over time, stop noticing it.
During auscultation of the heart, irregular tones of different loudness are heard. Arrhythmic pulse with different amplitude of pulse waves is determined. When atrial fibrillation is determined by the deficit of the pulse – the number of minute cardiac contractions exceeds the number of pulse waves). The lack of pulse is due to the fact that it is not at every heartbeat that blood is released into the aorta. Patients with atrial flutter feel palpitations, shortness of breath, sometimes discomfort in the region of the heart, pulsation of the veins of the neck.
Complications of atrial fibrillation
The most common complications of atrial fibrillation are thromboembolism and heart failure. In mitral stenosis complicated by atrial fibrillation, blockage of the left atrioventricular orifice with an intraatrial thrombus can lead to cardiac arrest and sudden death.
Intracardiac thrombi can enter the system of arteries of the pulmonary circulation, causing thromboembolism of various organs; Of these, 2/3 of the blood flow into the cerebral vessels. Every 6th ischemic stroke develops in patients with atrial fibrillation. The most susceptible cerebral and peripheral thromboembolism patients over 65 years; patients who have already had previous thromboembolism of any localization; suffering from diabetes, systemic arterial hypertension, congestive heart failure.
Heart failure with atrial fibrillation develops in patients suffering from heart defects and impaired ventricular contractility. Heart failure in mitral stenosis and hypertrophic cardiomyopathy can manifest as cardiac asthma and pulmonary edema. The development of acute left ventricular failure is associated with impaired emptying of the left heart, which causes a sharp increase in pressure in the pulmonary capillaries and veins.
One of the most severe manifestations of heart failure in atrial fibrillation may be the development of arrhythmogenic shock due to inadequately low cardiac output. In some cases, atrial fibrillation can be transferred to ventricular fibrillation and cardiac arrest. Chronic heart failure develops most often in atrial fibrillation, progressing to arrhythmic dilated cardiomyopathy.
Diagnosis of atrial fibrillation
Usually, atrial fibrillation is diagnosed by physical examination. Palpation of the peripheral pulse is determined by the characteristic disordered rhythm, filling and tension. During auscultation of the heart, irregular heart sounds are heard, significant fluctuations in their volume (the volume of the tone I following the diastolic pause varies depending on the size of the ventricular diastolic filling). Patients with the identified changes are sent to a cardiologist consultation.
Confirmation or clarification of the diagnosis of atrial fibrillation is possible using data from an electrocardiographic study. At atrial fibrillation on an electrocardiogram there are no teeth P registering reductions of auricles, and the ventricular QRS complexes are located chaotically. When atrial flutter is in place of the P wave, atrial waves are determined.
Using daily ECG monitoring, the heart rhythm is monitored, the form of atrial fibrillation, the duration of paroxysms, their connection with exercise, etc. are specified. Exercise tests (bicycle ergometry, treadmill test) are performed to detect signs of myocardial ischemia and when selecting antiarrhythmic drugs.
Echocardiography allows you to determine the size of the cavities of the heart, intracardiac thrombus, signs of lesions of the valves, pericardium, cardiomyopathy, to assess the diastolic and systolic functions of the left ventricle. EchoCG helps in making decisions about prescribing antithrombotic and antiarrhythmic therapy. Detailed visualization of the heart can be achieved with an MRI or MSCT of the heart.
A transesophageal electrophysiological study (CPECG) is performed to determine the mechanism of development of atrial fibrillation, which is especially important for patients who plan to undergo catheter ablation or implantation of a pacemaker (artificial pacemaker).
Prevention of atrial fibrillation
The purpose of primary prevention is the active treatment of diseases potentially dangerous in terms of the development of atrial fibrillation (hypertension and heart failure).
Measures of secondary prevention of atrial fibrillation are aimed at compliance with the recommendations on anti-relapse drug therapy, cardiac surgery, limiting physical and mental stress, refraining from drinking alcohol.