Treatment of atrial septal defects is only surgical. Indications for cardiac surgery is the identification of hemodynamically significant arteriovenous discharge of blood.
The optimal age for the correction of blemish in children is from 1 to 12 years. Surgical treatment is contraindicated in cases of high pulmonary hypertension with veno-arterial discharge of blood due to sclerotic changes in the pulmonary vessels.
In case of atrial septal defects, various methods of their closure are resorted to: closure, plastics using a pericardial flap or a synthetic patch under hypothermia and infrared conditions. X-ray endovascular occlusion of the atrial septal defect allows closing the openings of no more than 20 mm.
Surgical correction of atrial septal defects is accompanied by good long-term results: in 80-90% of patients normalization of hemodynamics and the absence of complaints are noted.
Atrial septal defect (ASD) – one or more holes in the septum separating the left and right atrial cavities, the presence of which causes abnormal blood loss, impaired intracardiac and systemic hemodynamics. In cardiology, atrial septal defect occurs in 5–15% of persons with congenital heart defects, and 2 times more often in women.

Along with defects of the interventricular septum, coarctation of the aorta, open arterial duct, atrial septal defect is among the most common congenital heart defects. Atrial septal defect may be an isolated congenital heart defect or be combined with other intracardiac anomalies: an interventricular septal defect, abnormal pulmonary vein drainage, mitral or tricuspid insufficiency.
Atrial septal defect is a congenital anomaly of the heart, characterized by the presence of an open connection between the right and left atria. Defect of the interatrial septum is manifested by shortness of breath, increased fatigue, lag in physical development, palpitations, pale skin, murmur in the heart, the presence of a “heart hump”, frequent respiratory diseases. Defect of the interatrial septum is diagnosed based on ECG, PCG, EchoX, cardiac catheterization, atriography, angiopulmonography. In case of an atrial septal defect, its closure is made, plastic or endovascular occlusion.
Causes of atrial septal defect
The formation of the defect is associated with the underdevelopment of the primary or secondary atrial septum and endocardial rolls in the embryonic period. Genetic, physical, environmental and infectious factors can lead to impaired organogenesis.
The risk of developing an atrial septal defect in an unborn child is significantly higher in those families where there are relatives with congenital heart defects. Cases of familial atrial septal defects in conjunction with atrioventricular block or underdevelopment of hand bones (Holt-Oram syndrome) are described.
In addition to hereditary conditions, viral diseases of a pregnant woman (rubella, chicken pox, herpes, syphilis, etc.), diabetes mellitus and other endocrinopathies, taking certain medications and alcohol during pregnancy, industrial hazards, ionizing radiation, gestational complications (toxicosis, threatened miscarriage, etc.).
Features of hemodynamics in atrial septal defect
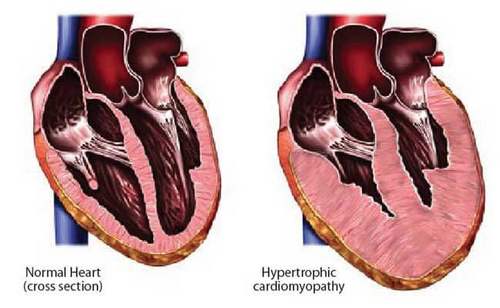
Due to the difference in pressure in the left and right atria, with atrial septal defect, arteriovenous shunting of blood from left to right occurs. The amount of discharge of blood depends on the size of the interatrial message, the ratio of the resistance of the atrioventricular orifices, the plastic resistance and the filling volume of the ventricles of the heart.
The left-right shunting of blood is accompanied by an increase in the filling of the pulmonary circulation, an increase in the volume load of the right atrium and an increase in the work of the right ventricle. Due to the discrepancy between the area of the valve opening of the pulmonary artery and the volume of release from the right ventricle, the development of relative stenosis of the pulmonary artery occurs.
Prolonged hypervolemia of the pulmonary circulation gradually leads to the development of pulmonary hypertension. This is observed only when pulmonary blood flow exceeds the norm by 3 times or more.
Pulmonary hypertension with atrial septal defect usually develops in children over 15 years of age, with late sclerotic changes in the pulmonary vessels. Severe pulmonary hypertension causes right ventricular failure and shunt change, which is manifested initially by transient venoarterial discharge (during exercise, straining, coughing, etc.), and then persistent, accompanied by constant cyanosis at rest (Eisenmenger syndrome).
Classification of atrial septal defects
Atrial septal defects differ in the number, size and location of the openings.
Taking into account the degree and nature of the underdevelopment of the primary and secondary interatrial septa, primary and secondary defects, as well as the complete absence of interatrial septum, causing a common, only atrium (three-chamber heart), respectively, are identified.
Cases of underdevelopment of the primary interatrial septum with preservation of the primary interatrial message are referred to the primary DMPP. In most cases, they are combined with splitting of the flaps of two- and tricuspid valves, open atrioventricular canal. The primary defect of the interatrial septum, as a rule, is characterized by a large size (3-5 cm) and is localized in the lower part of the septum above the atrioventricular valves and does not have a lower edge.
Secondary DMPP formed by the underdevelopment of the secondary septum. Usually they have small sizes (1-2 cm) and are located in the center of the interatrial septum or in the region of the mouths of the hollow veins. Secondary atrial septal defects are often combined with an anomalous pulmonary vein confluence into the right atrium. In this type of defect, the interatrial septum is retained in its lower part.
There are combined defects of the interatrial septum (primary and secondary, DMPP in combination with a defect of the venous sinus). Also, the defect of the interatrial septum can enter into the structure of complex CHD (triad and Fallot pentad) or be combined with severe heart defects – Ebstein’s anomaly, hypoplasia of the heart chambers, transposition of the great vessels.
The formation of a common (single) atrium is associated with an underdevelopment or the complete absence of primary and secondary partitions and the presence of a large defect that covers the entire area of the interatrial septum. The structure of the walls and both atrial ears are preserved. The three-chamber heart can be combined with abnormalities of the atrioventricular valves, as well as with asplenia.
One of the options for interatrial communication is an open oval window, due to the underdevelopment of its own valve oval orifice or its defect. However, since the open oval opening is not a true defect of the septum associated with the insufficiency of its tissue, this anomaly cannot be attributed to atrial septal defects.
Symptoms of atrial septal defect
Defects of the interatrial septum can occur with long-term hemodynamic compensation, and their clinic is characterized by considerable diversity. The severity of symptoms is determined by the size and location of the defect, the duration of the existence of CHD and the development of secondary complications. In the first month of life, the only manifestation of atrial septal defect is usually transient cyanosis with crying and anxiety, which is usually associated with perinatal encephalopathy.
With defects of the interatrial septum of medium and large sizes, the symptoms appear already in the first 3-4 months. or by the end of the first year of life and is characterized by persistent pallor of the skin, tachycardia, a moderate lag in physical development, insufficient weight gain.
For children with atrial septal defects, the typical occurrence of respiratory diseases is typical – recurrent bronchitis, pneumonia, occurring with prolonged wet cough, persistent dyspnea, abundant moist rales, etc., caused by hypervolemia of the pulmonary circulation. Children of the first decade of life have frequent dizziness, a tendency to fainting, fast fatigue, and shortness of breath on exertion.
Small defects of the interatrial septum (up to 10-15 mm) do not cause impairment of the physical development of children and characteristic complaints, therefore the first clinical signs of the defect can develop only in the second and third decades of life. Pulmonary hypertension and heart failure with atrial septal defect are formed by about 20 years, when there is cyanosis, arrhythmias, rarely – hemoptysis.
Diagnosis of atrial septal defect
An objective examination of a patient with atrial septal defect reveals pallor of the skin, a “heart hump”, moderate growth and weight lag. Percussion is determined by the increase in the boundaries of the heart left and right; during auscultation to the left of the sternum in the II-III intercostal spaces a moderately intense systolic murmur is heard, which, unlike the ventricular septal defect or pulmonary stenosis, is never gross. Above the pulmonary artery, splitting of the II tone and accentuation of its pulmonary component is detected. Auscultatory data are confirmed by phonocardiography.
In secondary defects of the interatrial septum, ECG changes reflect an overload of the right heart. Incomplete blockade of the right bundle of His, AV-blockade, sick sinus syndrome can be registered. Radiography of the chest organs makes it possible to see an increase in the pulmonary pattern, protrusion of the pulmonary artery trunk, and an increase in the shadow of the heart due to hypertrophy of the right atrium and ventricle. With fluoroscopy, a specific symptom of atrial septal defect is found – increased pulsation of the roots of the lungs.
An echocardiography study with color Doppler mapping reveals a left-right blood discharge, the presence of atrial septal defect, allows to determine its size and localization. When sounding the cavities of the heart, an increase in blood pressure and oxygen saturation in the right heart and pulmonary arteries is detected. In the case of diagnostic difficulties, the examination is supplemented with atriography, ventriculography, jugular vein phlebography, angiopulmonography, and MRI of the heart.
Atrial septal defect should be differentiated from ventricular septal defect, open arterial duct, mitral insufficiency, isolated pulmonary artery stenosis, Fallot triad, anomalous pulmonary vein confluence into right atrium.
Predisposition of interatrial septal defect
Minor atrial septal defects are compatible with life and can be detected even in old age. In some patients with a small atrial septal defect, spontaneous opening of the opening is possible during the first 5 years of life.
The life expectancy of persons with major defects of the interatrial septum with the natural course of the defect averages 35-40 years. The death of patients can occur from right ventricular heart failure, cardiac arrhythmias and conduction (paroxysmal tachycardia, atrial fibrillation, etc.), less often from a high degree of pulmonary hypertension.
Patients with atrial septal defects (operated and non-operated) should be monitored by a cardiologist and a cardiac surgeon.



Are you tired? I’m worried about you. Please be ok!
Yes- society better not ignore problem any longer. How to proceed?