Complex therapy of the disease includes the cessation of the use of ethanol-containing drinks, the fight against heart failure, the correction of metabolic disorders, the restoration of the functions of other organs.
A positive effect from the course of treatment is possible at an early stage of the disease in the absence of irreversible disorders.
In the later stages, continuous medication is required.
The following areas of treatment for cardiomyopathy are distinguished:
- Lifestyle change. Provides a complete waiver of alcohol, the exclusion of smoking. Assigned to a diet with plenty of protein, restriction of salt and fat. Preference is given to steamed, stewed or boiled dishes, food is carried out in small portions 4-6 times a day. Daily fluid intake is not more than 1.5 liters. Adequate exercise, healthy sleep, stress reduction are important.
- Drug therapy. Is the basis of the treatment of the disease, involves the use of several groups of drugs that are prescribed individually, taking into account the symptoms. Antihypertensive drugs are used to normalize blood pressure, antiarrhythmics are used to prevent rhythm disturbances, diuretics are used to eliminate edema, and statins are used to lower blood cholesterol. In severe cases, the treatment plan is supplemented with cardiac glycosides to relieve attacks of tachyarrhythmias, antiplatelet agents and anticoagulants to prevent thromboembolic complications.
- Surgical intervention. With the ineffectiveness of conservative therapy, the rapid progression of alcoholic cardiomyopathy with a high risk of developing dangerous complications, the issue of heart transplantation is being considered. The method provides a high 10-year survival rate (about 75%), is used in a satisfactory condition of the body, in the absence of gross mental and intellectual disorders. The disadvantages of the technique are the invasiveness, high cost, lack of donor organs.
Alcoholic myocardial damage is a common cause of cardiomyopathy. The incidence is determined by the prevalence of alcoholism in the population. The disease often develops in middle-aged people who systematically use alcohol for a long time. Among patients, there is a predominance of males.
The probability of pathology increases with smoking, stress, the presence of other factors contributing to the occurrence of heart and vascular diseases. Alcoholic cardiomyopathy accounts for at least 30% of cases of dilated cardiomyopathy.
Causes of alcoholic cardiomyopathy
The main etiofactor is prolonged consumption of large amounts of alcoholic beverages, usually in the equivalent of 100 ml of pure ethanol every day for 10-20 years (according to statistics, in Russia the average alcohol consumption per person per year is from 11 to 14 liters or about 35 -40 ml per day).
The disease is diagnosed in 50% of chronic alcoholics. The factors contributing to the occurrence of cardiomyopathy include hereditary predisposition, immune disorders, poor nutrition, chronic stress, overwork, smoking.
Pathogenesis of alcoholic cardiomyopathy
Toxic effects of alcohol metabolism, primarily acetaldehyde, have a negative impact on the myocardium. This substance is formed by the liver cells after the breakdown of ethanol and then enters the bloodstream. Reaching the heart, it causes structural and functional disorders: it negatively affects the reproduction of the contractile proteins of the heart muscle, reduces its strength, and disrupts the metabolism inside the cardiomyocytes (the transport of lipids, potassium, calcium).
Metabolic disorders and electrolyte imbalance cause arrhythmias, a decrease in the functional activity of the heart, and the development of fibrotic changes. There is evidence that acetaldehyde affects the synthesis of certain compounds, in particular, it stimulates the production of pro-inflammatory cytokines and proteins that can provoke an autoimmune response.
In addition, with a high blood content, ethanol and various substances added to alcoholic beverages – metal impurities (for example, cobalt), dyes, and preservatives – may have a direct toxic effect on the heart.
Classification of alcoholic cardiomyopathy
Systematization of types of alcoholic cardiomyopathy is carried out taking into account the characteristics of clinical symptoms, the severity of certain manifestations. The division is rather arbitrary, since the symptoms of the disease differ in variability – the symptoms corresponding to different types of the disease can be detected in one patient.
There are four forms of pathology:
- Classic. Heart failure dominates the clinical picture. When alcohol consumption is stopped, there is a positive clinical and echocardiographic dynamics, the longer the period of abstinence lasts, the better the patient’s condition becomes. The resumption of admission leads to a rapid deterioration of the condition, the reappearance and aggravation of symptoms.
- Pseudo-ischemic. The main manifestation is stitching or aching pains in the cardiac area in the presence of ECG changes characteristic of coronary heart disease. Cardialgia occurs after drinking alcohol, is not associated with physical exertion, not quenched by nitroglycerin. The severity of symptoms gradually progresses.
- Arrhythmic. The clinic is dominated by cardiac arrhythmias. Atrial fibrillation is detected in 20% of patients, arrhythmia, tachycardia, atrial flutter, or atrial fibrillation are less common. A feature of the arrhythmias of alcoholic etiology is their occurrence after a massive intake of ethanol-containing beverages. Rhythm disturbances can be the first and often the only symptom of cardiomyopathy.
- Mixed Combines the manifestations of all previous variants of myocardial damage. It is considered the most unfavorable, since the symptoms mutually aggravate each other, which significantly worsens the prognosis of the disease. In 30–40% of patients with this type of cardiomyopathy, signs of susceptibility to severe ventricular arrhythmias and sudden cardiac death are detected on an ECG.
Symptoms of alcoholic cardiomyopathy
The onset of the disease is characterized by nonspecific manifestations that occur as a result of functional disorders in the activity of various organs and systems 4-5 years after the systematic use of large volumes of alcoholic beverages. Patients complain of fatigue after minor physical exertion, weakness, drowsiness, and increased sweating. With intense load may be prolonged pain in the chest, in the neck.
Rhythm disturbances are represented by extrasystole, tachycardia, a feeling of a sinking heart. Vegetative disorders include feeling hot, trembling hands, facial redness, agitation, or lethargy. Symptoms usually appear the day after alcoholic excesses. In the period of abstinence from alcohol, the intensity of the manifestations decreases. Symptoms may persist for up to 10 years.
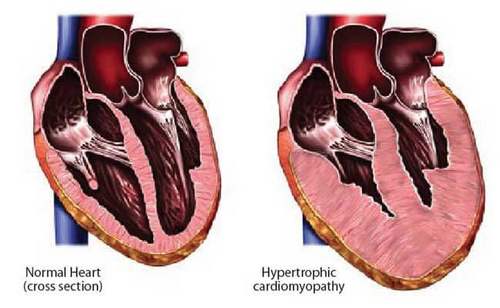
With the continuation of the systematic consumption of ethanol-containing beverages, myocardial hypertrophy develops, which is quickly replaced by dilatation. The chambers of the heart expand, their contractile ability decreases, which causes heart failure, blood stagnation in the small and large circulation. There is persistent dyspnea, to the clinical picture of the disease are added asthma attacks at night, edema of the lower extremities, cough (dry or with a small amount of light sputum). Can turn out cyanosis, cold hands, legs.
In the absence of treatment, irreversible structural changes in the internal organs develop on the background of cardiomyopathy. Due to circulatory disorders, the kidneys function is disturbed, toxic products of metabolism accumulate in the body, which adversely affect the activity of the central nervous system and internal organs. The defeat of the nervous system leads to encephalopathy, manifested by a decrease in cognitive functions, unmotivated aggression, bitterness, an unsteady gait, and sleep disorders. At the terminal stage, there are gross violations of the nervous system, progression of heart, kidney and liver failure, leading to the death of the patient.
Complications of alcoholic cardiomyopathy
With alcoholic myocardial damage, there is a high risk of complications, including life-threatening ones. The most common consequence is a critical rhythm disturbance – ventricular fibrillation, which is characterized by ineffective contractions and without cardiovascular care leads to cardiac arrest.
Against the background of functional insufficiency of the heart muscle, blood flow in the chambers slows down, its rheological properties are disturbed, the likelihood of thromboembolic complications increases with the development of stroke, myocardial infarction, acute renal failure, and necrosis of various gastrointestinal tracts.
Diagnosis of alcoholic cardiomyopathy
This pathology is diagnosed by a therapist or cardiologist. Since patients often conceal the fact of alcohol abuse, if alcoholic cardiomyopathy is suspected, the relatives of patients are questioned, if an appropriate etiology is identified, they advise a narcologist to select the optimal treatment strategy for addiction.
The list of diagnostic measures includes:
- Objective examination. Restless or inhibited behavior, cyanosis of the tips of the fingers, nose, ears, upper chest can be detected. On palpation, there is increased sweating, swelling and cooling of the limbs, swelling and pulsation of the neck vessels. An increase in the size of the heart during percussion indicates hypertrophy or dilatation of its chambers. Auscultation determines the pathological noise characteristic of structural changes in the myocardium, valves.
- Electrocardiography. It is a basic instrumental method of research, allows to detect rhythm disturbances, to obtain data on organic lesion of the myocardium, to suggest its toxic etiology. The ECG can be supplemented with daily Holter monitoring. In the absence of contraindications appoint bicycle ergometry.
- Echocardiography. EchoCG is used to assess the condition of the coronary arteries and the valvular apparatus, detect hypertrophy and myocardial dilatation, reduce blood flow velocity, determine the pressure in the chambers. It is performed for the differential diagnosis of cardiomyopathy and pericarditis.
- X-ray OGK. On chest radiographs, signs of an enlarged chambers of the heart are visualized, rarely dilatation of the ascending aorta. The technique is used to clarify the status of other large vessels, identify pathological formations. Based on the pictures, valve defects can be suspected.
Differential diagnosis of alcoholic cardiomyopathy is carried out with diseases with a similar clinical picture: angina, ischemic heart disease, myocardial infarction, dissecting aortic aneurysm, pleurisy, pneumonia. Other types of cardiomyopathy are excluded: restrictive, hypertrophic, arrhythmogenic dysplasia of the right ventricle.
Prognosis and prevention of alcoholic cardiomyopathy
In the early stages of the disease, subject to the complete rejection of alcohol and the timely start of treatment, the prognosis is favorable. With the development of irreversible changes in the heart muscle, there is a significant reduction in life expectancy.
Prevention of cardiomyopathy is not only a medical but also a social task; it includes measures to combat alcoholism: informing the population about the basic principles of a healthy lifestyle, restricting advertising of alcoholic beverages and their distribution among young people at the legislative level.
Preventive measures also involve bringing to the public information about the consequences of prolonged alcohol intoxication, its effects on the heart, other organs and systems.



