Despite the fact that an attack of cardiac asthma can be stopped on its own, due to the high risk of pulmonary edema and a threat to the life of the patient, emergency medical care is needed on the spot.
Conducted therapeutic measures should be aimed at suppressing the neuro-reflex excitation of the respiratory center, reducing emotional stress and unloading the pulmonary circulation.
To facilitate the course of an attack of cardiac asthma, the patient needs to ensure maximum rest, a comfortable semi-sitting position with his legs flattened, and a hot foot bath should be organized.
Subcutaneous administration of nitroglycerin is indicated with repetitions every 5–10 min. or nifedipine with mandatory monitoring of blood pressure to subjective relief of the condition.
In cardiac asthma with severe dyspnea and pain syndrome, narcotic analgesics are used. In the case of respiratory depression, bronchospasm, chronic pulmonary heart, brain edema, they can be replaced by neuroleptanalgetic – droperidol.
Bleeding (300-500 ml of blood) is the method of emergency unloading of the pulmonary circulation in case of arterial hypertension and venous congestion. In the absence of contraindications, it is possible to apply a tourniquet on the limbs, which squeezes the veins and artificially creates venous stagnation on the periphery (lasting no more than 30 minutes under the control of an arterial pulse). In cardiac asthma, prolonged repeated inhalations of oxygen through ethanol are shown (using nasal catheters or masks, and in pulmonary edema, mechanical ventilation), which help to reduce pulmonary edema.
With the development of an attack of cardiac asthma, blood pressure is corrected by antihypertensive drugs and diuretic drugs (furosemide). In almost all cases of cardiac asthma, intravenous injection of cardiac glycosides solutions – strophanthin or digoxin is necessary. Euphyllinum can be effective in mixed form of asthma, cardiac and bronchial, with mitral stenosis due to the expansion of the coronary vessels and improve the blood supply to the myocardium. In cardiac asthma with cardiac rhythm disturbances, electropulse therapy (defibrillation) is used. After stopping an attack of cardiac asthma, further treatment is carried out taking into account the cause of the disease.

Cardiac (cardiac) asthma is a clinical syndrome characterized by sudden attacks of inspiratory dyspnea developing into asphyxiation. In cardiology, cardiac asthma refers to severe manifestations of acute failure of the left heart, complicating the course of a number of cardiovascular and other diseases. In cardiac asthma, there is a sharp decrease in the contractility of the myocardium and blood stasis in the system of the pulmonary circulation, leading to acute disorders of respiration and blood circulation. Cardiac asthma can precede the development of alveolar pulmonary edema (often fulminant), often resulting in death.
Cardiac asthma is an acute left ventricular failure caused by stagnation of blood in the pulmonary circulation and interstitial pulmonary edema. Attacks of cardiac asthma are accompanied by a feeling of acute lack of air, orthopnea, heavy dry cough, facial cyanosis, tachycardia, increased diastolic blood pressure, agitation, and fear of death. The diagnosis of cardiac asthma is based on the assessment of clinical symptoms, examination data, anamnesis, chest X-ray, ECG. An attack of cardiac asthma is stopped by using nitroglycerin, narcotic analgesics, hypotensive and diuretic drugs, bleeding, the imposition of venous plaits on the limbs, oxygen therapy.
Causes of Cardiac Asthma
Cardiac asthma may be associated with direct damage to the heart or develop on the background of non-cardiogenic diseases and conditions. The causes of cardiac asthma may be primary acute or chronic (in the acute stage) left ventricular failure.
Cardiac asthma can complicate the course of various forms of ischemic heart disease (including acute myocardial infarction, unstable angina), post-infarction and atherosclerotic cardiosclerosis, acute myocarditis, postpartum cardiomyopathy, cardiac aneurysm. Paroxysmal forms of arterial hypertension with high blood pressure rises and excessive voltage of the left ventricular myocardium, attacks of atrial fibrillation and atrial flutter are potentially dangerous in terms of the development of cardiac asthma.
Cardiac asthma is often caused by decompensated mitral and aortic heart defects (mitral stenosis, aortic insufficiency) associated with an obstacle to blood outflow. The presence of a large intraatrial thrombus or intracavitary heart tumor, myxoma, can contribute to impaired blood flow in the left parts of the heart.
The development of cardiac asthma can cause infectious diseases (pneumonia), kidney damage (acute glomerulonephritis), an acute violation of cerebral circulation. The factors provoking the onset of an attack of cardiac asthma include inadequate physical exertion, severe emotional stress, hypervolemia (when a large amount of fluid is administered intravenously or delayed, fever, pregnancy), abundant food and fluid intake at night, switching to a horizontal position.
Pathogenesis of cardiac asthma
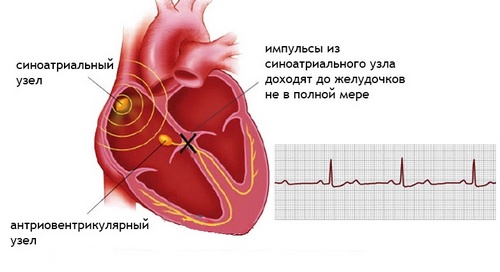
The mechanism of development of an attack of cardiac asthma is associated with the difficulty of intracardiac hemodynamics in the left parts of the heart, leading to excessive blood supply to the pulmonary veins and capillaries and a sudden increase in hydrostatic pressure in the pulmonary circulation.
Due to an increase in the permeability of the capillary walls, there is an active release of plasma into the lung tissue (primarily in the perivascular and peribronchial spaces) and the development of interstitial pulmonary edema. This impairs the ventilation of the lungs and impairs the normal gas exchange between the alveoli and the blood.
A certain role in the development of the clinical symptoms of cardiac asthma is played by the neuro-reflex links in the regulation of respiration, the state of the cerebral circulation.
Vegetative symptoms accompanying an attack of cardiac asthma develop when the respiratory center is excited as a result of its blood supply failure or reflex, in response to impulses from various foci of irritation (for example, from the aortic root).
Heart Asthma Symptoms
The precursors of an attack of cardiac asthma may include shortness of breath, constriction in the chest, coughing with a little physical exertion or going into a horizontal position. Attacks of cardiac asthma are more often observed at night, during sleep due to the weakening of adrenergic regulation and an increase in blood flow to the small circle system in the prone position. In the daytime, an attack of cardiac asthma is usually associated with physical or neuro-psychological stress.
Typically, attacks of cardiac asthma occur suddenly, forcing the patient to wake up from a sense of acute lack of air and an increase in shortness of breath, turning into asphyxiation and accompanied by a hacking dry cough (later with a small amount of clear sputum). During an attack of cardiac asthma, it is difficult for the patient to lie down, he assumes a forced upright position: he gets up or sits in bed, having lowered his legs down (orthopnea); usually breathes through the mouth, speaks with difficulty.
The condition of the patient with cardiac asthma is agitated, restless, accompanied by a sense of panic fear of death. On examination, cyanosis is observed in the region of the nasolabial triangle and nail phalanges, tachycardia, and an increase in diastolic blood pressure. On auscultation, dry or scanty fine bubbling rales may occur, mainly in the lower parts of the lungs.
The duration of an attack of cardiac asthma can be from several minutes to several hours, the frequency and characteristics of the manifestation of attacks depend on the specifics of the underlying disease. In mitral stenosis, attacks of cardiac asthma are rarely observed, since the reflex constriction of pulmonary arterioles (Kitayev’s reflex) prevents stagnation in the capillaries and the venous bed of the pulmonary circulation.
With the development of right ventricular insufficiency, attacks of cardiac asthma can disappear altogether. Sometimes cardiac asthma is accompanied by reflex bronchospasm with impaired bronchial patency, which complicates the differential diagnosis of the disease with bronchial asthma.
With a prolonged and severe attack of cardiac asthma, “gray” cyanosis appears, cold sweat, swelling of the neck veins; pulse becomes filiform, pressure drops, the patient feels a sharp decline in strength. Transformation of cardiac asthma into alveolar pulmonary edema can occur suddenly or in the process of increasing severity of the disease, as evidenced by the appearance of abundant foamy, sputum mixed with blood, moist fine and medium bubbly rales over the entire surface of the lungs, severe orthopnea.
Diagnosis of cardiac asthma
For the proper prescription of drug therapy, it is important to differentiate an attack of cardiac asthma from a choking attack in bronchial asthma, acute laryngeal stenosis, from dyspnea in uremia, mediastinal syndrome, and hysterical seizure. An assessment of the clinical manifestations of cardiac asthma, an objective physical examination, anamnesis, chest radiography, an ECG can help establish an accurate diagnosis.
Auscultation of the heart during an attack of cardiac asthma is difficult due to the presence of breathing noises and wheezing, but still allows you to identify deafness of heart sounds, canter rhythm, accent II tone of the pulmonary trunk, as well as signs of the underlying disease – disturbance of heart rhythm, failure of heart valves and aorta and others. There is a frequent, weak filling of the pulse, an increase, and then a decrease in blood pressure. When listening to the lungs, single or scattered dry (sometimes single wet) wheezing are determined.
Radiographs of the chest in cardiac asthma show signs of venous congestion and plethora in the small circle, a decrease in the transparency of the lung fields, expansion and blurring of the roots of the lungs, the appearance of Curly lines indicating interstitial pulmonary edema. On an ECG, during a heart attack of asthma, a decrease in the amplitude of the teeth and the ST interval is observed, arrhythmias and signs of coronary insufficiency may be recorded.
In cardiac asthma, which occurs with reflex bronchospasm, an abundance of wheezing and increased secretion of sputum, in order to exclude bronchial asthma, the age of the first manifestation of the disease (in cardiac asthma – old age), the patient’s absence of allergic history, chronic inflammatory diseases of the lungs and upper respiratory tract are taken into account, the presence of acute or chronic cardiovascular disease.
Prognosis and prevention of cardiac asthma
The outcome of cardiac asthma is largely determined by the underlying pathology leading to the development of asthma attacks. In most cases, the prognosis of cardiac asthma is poor; sometimes complex treatment of the underlying disease and strict adherence to a restrictive regimen in patients allow preventing recurrent seizures, maintaining a relatively satisfactory condition and even working for several years.
Prevention of cardiac asthma is the timely and rational treatment of chronic coronary artery disease and heart failure, hypertension, the prevention of infectious diseases, compliance with water-salt regimen.