Prolapse (prolapse) of intervertebral disk – hernia intervertebral disk. The latter are placed between the vertebrae and act as a cushion or shock absorbing apparatus, another function of their maintaining flexibility and strength of the spine.
Made of fibrous connective tissue, connecting with a Central jelly-like core. In the middle of the column is localized to the spinal cord. And megapotamicum space are nanocores.
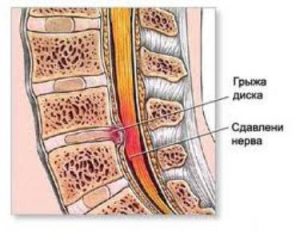
The disease develops when the outer fibers of the ring injured, the soft tissue called the nucleus pulposus breaks away from its private space. Tearing or prolapse of disc material can be introduced into the spinal canal leads to compression of the spinal cord, however, often undergo the pressure of the spinal nerves.
Postprocess rarely formed in the child’s body, it is found mainly in the medium to young age group. Sometimes develops suddenly, is dependent on the degree of protrusion or gradual manner over a number of weeks or months.

In accordance with statistical information about 45-49% of the area between the lumbar and the sacral division (L4-L5-S1).
Causal factors
The main reason for the formation of postprocess can be excessive pressure and load in the affected area:
- Falling from a great height. Creates unnecessary pressure on the spine, in the case of increased power, combined with the injury to the vertebra is a high probability of prolapse.
- Bending in front side when fiznagruzki. When a person bends over and tries to lift too heavy an object, the pressure can contribute to tearing of the intervertebral annulus fibrosus.
- Serial accidental fractures of the vertebrae, which are critical and not bring strong damage, however, later during a low pressure in the vertebral area may develop protrusions. Described develops as a result of weakness of the outer fibers of the vertebra.
The disease could also be two methods:
- Direct pressure. The disk is formed with a gap in the spinal canal or intervertebral hole is able to compress neural roots.
- Chemical irritation. In the kernel includes a number of components, called “inflammatory mediators.” The latter contribute to the chemical irritation narokoroko, leading to an inflammatory process in the nerves.
Often fixed prolapse in lumbar (L4-L5 ) and cervical area (C5-C6). And uncommon in the thoracic spine, because it is the most protected mysecretkey a corset.
The main reasons for the defeat lumbalna-sacral division:
- Low back pain – decrease the width of the disks due to the degeneration and dystrophy (disorder krovoobrascheniya).
- Injury of the spine with the violation of the integrity of the lumbar or sacral segments.
- Autoimmune disease.
- Connective tissue diseases of inflammatory Genesis.
- Viral and bacterial phenomena, intoxication, etc.
Symptomatic picture
In practical terms, the basic manifestation of the prolapse protrudes painful syndrome that consists of:
- pain with irrationalism in both upper extremities;
- pain in tibialis or gluteal region depends on the injury;
- a feeling of numbness, pricking or tingling in the upper and lower extremities;
- mikaboshi in the implementation of motor acts with hands or feet.
In severe clinical picture characteristic of loss of control of the bladder or bowel, a severe numbness in the genital area. Localization of the described features has direct dependence on the painful area. The more painful point, the easier it is to diagnose.
Diagnosis
Diagnosis begins with a complete collection of anamnestic information and often completes the physical examination. The next stage performs clinical diagnosis, which provides information about localization and precision of the development of prolapse.
Depending on the symptomatic picture perform the following tests:
- Local radiographic examination. Assigned to determine pathological focus in the spinal column or degenerative transformations in the damaged region.
- MRI. Apply for a detailed assessment of the state of the spinal tissue and spinal discs.
- Electrophysiological examination to determine damage to nerve fibers.
- Discograficas examination of the painful syndrome.
Therapeutic interventions
In the absence of instrumental diagnosis of inflammation in the spinal cord or compression of a nerve root provides for medicinal treatment. Often used combination Antimonopoly drugs (NSAIDs) fizioterapevticheskoe program, or therapy and Pilates.
In the case of ineffectiveness of medication (tablet method) of treatment prescribed injection rate, including local anesthesia.
In acute process in some cases, resort to surgical intervention to prevent recurrent symptoms.
Neurosurgical treatment is required is selected based on clinical manifestations, radiographic information, and external factors.



