Argentine hemorrhagic fever – natural-focal zoonoses group of the South American hemorrhagic fevers caused by RNA – containing virus Junin. Leading clinical manifestations are hemorrhagic syndrome with bleeding of different localization, severe intoxication.
Diagnosis is based on detection of the pathogen and specific markers in the blood serum.
Causative treatment involves injection of immune plasma. Good results shows the assignment of ribavirin. Given the evolved violations are assigned symptomatic therapy.
Argentine hemorrhagic fever
Focus of hemorrhagic fever Junin is the wet ecosystem of the pampas of Argentina. Outbreaks occur annually from February to June with a peak in may. Most common in men, infection is more common among the rural population. A large part of the patients are people of working age. Each year, on average affects up to 4,000 people, during outbreaks the number of infected could reach 20,000. About 10% of the local population are seropositive without manifestation of the infection in history.
Because active immunization of residents of this region in recent times manage to control the incidence with a decrease in the frequency of episodes with severe. Since this vaccination is not included in the list of required upon entry to Argentina, cases of infection of tourists.
Causes of Argentinean hemorrhagic fever
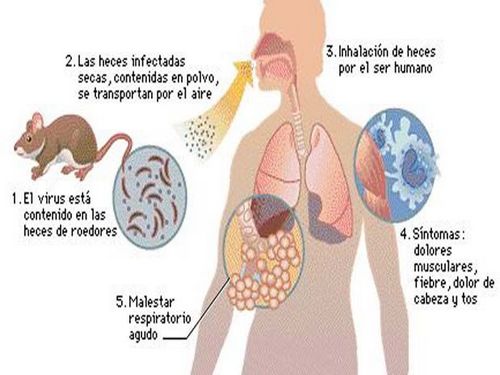
The pathogen – RNA-containing Junin virus of the genus Arenavirus of the family Arenaviridae. The virus dies under the influence of detergents, ultraviolet irradiation, however, has long maintained in lyophilized state. Reservoir and source of infection are rodents homalopsinae and sick man. Between the rodents and the pathogen is transmitted transmissive biting gamanovich mites. Penetrating into the blood, the virus in hamsters causes a latent course of the disease and asymptomatic viremia. The pathogen from the body of rodents is excreted in the urine.
In the human organism infectious agent enters by inhalation of dust inhalation of dust contaminated with rodents, as well as during the realization of fecal-oral mechanism with contaminated food and water, through sexual contact and through damaged skin. The bite of a tick infected with the virus, the disease in humans does not develop. Annually vnutrikoronarnogo describes the cases of infection by aspiration with the development manifested forms or asymptomatic course. After the disease formed a strong immunity.
Pathogenesis
The mechanism of development of Argentine hemorrhagic fever is not fully understood. Once in the alveolar macrophages and bronchopulmonary lymph nodes, Junin virus from blood and lymphokine spreads throughout the body. The pathogen is recorded in the cells of the reticuloendothelial system, damaging them, thereby contributing to leuko – and thrombocytopenia. Develops lymphadenopathy, lymphoid follicles observed atrophy, necrosis.

Damage to the capillary walls leads to the emergence of hemorrhagic syndrome, hypovolemic shock. Damage to the blood vessels of internal organs contributes to the violation of their functions. Depending on viral load can develop as asymptomatic with the increase in antibody titer and severe condition.
The symptoms of Argentinean hemorrhagic fever
The incubation period after infection is approximately 7-14 days. The disease begins gradually, appear nonspecific symptoms: fever, weakness, malaise, headache, arthralgia, myalgia. For a short period of time the body temperature rises to febrile digits, there is anathema in the conjunctiva, oral mucosa. Objectively determined the reddening of the face, neck, injection of vascular sclera, lymphadenopathy, rarely may appear hemorrhagic rash. For the first phase of disease is characterized by bradycardia, often develops myocarditis.
The duration of febrile period is about 10 days. Then manifest the symptoms of hemorrhagic syndrome: increased bleeding of the gums, marked epistaxis, hematuria, melena. Blood pressure falls to 60 mm Hg. century, when massive bleeding develops hemorrhagic shock. May cause symptoms of CNS injury with increasing neurological deficit (agitation, stupor, signs of encephalitis). The recovery period ranges from 2 weeks to several months.
Complications
The most frequent complication is hemorrhagic shock. When shock is severe likely to develop multiple organ disorders (acute renal, cardiac, respiratory insufficiency). In addition, possible CNS lesions of different character attach neurologic syndromes (encephalopathy, encephalitis). In vaccinated patients after previous infection sometimes appears transient alopecia. Quite often on the background radiation and damage to the capillary walls occur pneumonia. The most common cause of death is pulmonary edema. In connection with the introduction of vaccine prevention of severe forms of the disease are becoming increasingly rare.
Diagnosis
In cases of suspected hemorrhagic fever it is necessary to consult infectious disease with subsequent hospitalization in a patient in an intensive care unit hospital for infectious diseases. During the physical examination specific symptoms for this virus infection are not observed. Noteworthy obscheintoksikatsionnogo syndrome, redness, swelling of neck, face, and perhaps the presence of petechial rash, lymphadenopathy. Characterized by the appearance of conjunctivitis, enantemy on the oral mucosa.
In diagnostics use the following clinical laboratory methods:
- General and biochemical material. Due to damage to the cells of the reticuloendothelial system in the KLA reported the presence of thrombocytopoiesis and radiation. Due to the defeat of the vascular wall and extravasation the liquid portion of blood is showing signs of thickening of blood. In General, the analysis of urine – proteinuria. Daily loss of protein in the urine can reach 10 g. the appearance of multiple organ failure in the blood increase the relevant markers (Alt, AST, urea, creatinine).
- Detection of infectious agents. For the detection of specific antibodies in the blood is taken after 2 weeks from the onset of the disease. This method is rather retrospective. Using the complement fixation, indirect immunofluorescence reaction, reaction of braking of hemagglutination. For detection of virus examined pharyngeal swabs, urine; fence produce up to 7 days from the onset of the disease. The most sensitive method for detection of the pathogen in the early stages is PCR with reverse transcription.
Given the relative rarity of the disease outside endemic areas and non-specificity of the initial symptoms, the diagnosis can cause considerable difficulties. The differentiation is from other haemorrhagic fevers, in particular, with South American (Bolivian, Venezuelan, Brazilian). In the stage of intoxication in the absence of a pronounced hemorrhagic syndrome is necessary to exclude influenza, arbovirus infections, sepsis, and in the midst of disease – hemorrhagic diathesis. The elucidation of the history of the disease and comparison of clinical data with the results of tests allows to establish the correct diagnosis and prescribe appropriate treatment.
Treatment of Argentine hemorrhagic fever
Treatment must be carried out in isolation of the patient under the control of an infectious disease physician. When joining complications may need to consult specialists (neurologist, pulmonologist, nephrologist, cardiologist). Is necessary to observe strict bed rest. The main method of therapy is the transfusion of convalescent plasma. The best results this method gives for the early stages of the disease (up to 8 days).
There are data about the positive results of treatment with ribavirin. This method is particularly relevant in the absence of immune plasma. According to the who guidelines, the drug is administered intravenously on the first day in a dose of 30 mg/kg once, then 15 mg/kg 4 times/day. 4 days and 7.5 mg/kg/day. 6 days. Parallel to symptomatic treatment with correction of disorders developed (detoxification therapy, recovery of the blood volume, the use of cardiovascular tools, antipyretic drugs, correction of disorders of hemostasis).
Prognosis and prevention
At the time the disease is recognized and proper treatment the prognosis is favorable. In the case of severe forms of the duration of the Argentine hemorrhagic fever is about 11 hours, and mortality reaches 15%. Activities of nonspecific prevention includes rodent control in endemic areas through the use of poisons, traps. In addition, requires the use of respirators to dust.
Vaccination of local residents allows you to monitor the course of disease. Today attenuating use a live vaccine, being tested experimental samples. The use of ribavirin as an emergency prophylaxis is not recommended. With the exception of pregnant patients in contact with the patient.



