Allergic rhinitis or rhinitis in the child and the adult – is a disease of inflammatory nature, characterized by allergic reactions in the mucous sheathlining the cavity of the nose.
In the result, the epithelium of the mucous membrane swells, rhinorrhea occurs, i.e. increased production of mucus, paroxysmal sneezing, nasal congestion. You must know how to distinguish allergic rhinitis from the common cold because the treatment is different.
Characteristic symptoms of allergic rhinitis can be learned from the proposed article also presents standards for the treatment of this pathology.
The disease is widespread in our country, among various age and social segments of the population, in particular, and in young children. This is one of the most common diseases that is diagnosed in 10-25% of the adult population. In children of school age, the disease occurs in one in 100 people. Children under one year of age an not get sick.
One type of allergic rhinitis – hay fever or pollinosis, seasonal allergie.
Causes of allergic rhinitis and sneezing
Allergic rhinitis and sneezing are one main cause – exposure of allergen, which could be exposed not only through inhalation of air and contact with skin cells, but also with food, with water, without direct contact with the mucosa.

Causes of seasonal (temporary) of allergic rhinitis, i.e. hay fever, the allergens are plant pollen that gets into the respiratory tract with air. This usually occurs in the period of flowering grasses, trees, flowers. Especially dangerous in relation to allergic reactivity such plants as ragweed, which blooms in the country, birch, poplar, quinoa, cereals, walnuts.
Perennial allergic rhinitis occurs due to sensitization to other allergens:
- dust mites and fungus of dust, slomannye the epidermis, hair and fluff Pets, including fluff out of pillows, blankets, outerwear, toys, book dust
- components of tobacco smoke, exhaust gases, chemicals and industrial manufacturing, production chemical hazard
- detergents and cosmetics (surfactants, detergents, fragrances, antistatic agents, essential oils, dyes)
- natural and chemical food allergens (honey, citrus, egg white, colorful vegetables and fruits, cocoa, nuts, sea food, sweets, milk, conservatry, meats, food colorings, flavorings, preservatives)
- drugs: penicillin etc.
Allergic rhinitis in a child
Many parents mistakenly believe that allergic rhinitis the child does not require special treatment and resolves on its own with age. In fact it is not. Untreated allergosis leads to habituation of the immune system to pathological responses, its depletion and the formation of persistent pathological response to allergen. In other words, over time, long-existing Allergy to become chronic in the future becomes resistant to treatment. Which greatly increases the risk of developing other, more severe allergic diseases, such as obstructive bronchitis and bronchial asthma.
Therefore, to ensure the child’s health in the future should immediately begin treatment of any allergies and provide the body for some time hypoallergenic regime.
At the beginning of the appearance of Allergy there are many chances with the help of a competent treatment to restore the normal response of the immune system, prevent recurrence and to protect the child from severe chronic diseases in adulthood. To do this, take the baby for a consultation at the doctor and strictly to implement the resulting recommendations.
The symptoms of allergic rhinitis
To suggest allergicheskie cold, pay attention to specific symptoms.

There are three degrees of severity of an:
- mild: symptoms do not bring a marked discomfort to the patient and do not affect his quality of life and ability to work, does not violate sleep
- average degree: manifestations of rhinitis cause minor or temporary discomfort, and can reduce the capacity to interfere with sports training, to disturb the sleep
- severe: symptoms are significantly expressed, lead to a significant breach of disability and quality of life, causing a sharply unpleasant sensations
Rhinitis begins suddenly after contact with an allergen, and is a frequent paroxysmal sneezing, profuse rhinorrhea, that is, the discharge from the nose watery transparent liquid, odorless, edema and stuffy nasal passages, until the complete cessation of nasal breathing.
Sometimes the above symptoms are other signs of an allergic reaction: redness and itching of the skin and mucous membranes, rash, allergic-type hives, watery eyes, swelling of the face, redness of the eyelids, impaired sense of smell.
When a permanent form of rhinitis symptoms can be blurred, dull, intermittent, and limited to a small stuffy nose and sneezing. Most often sudden and striking manifestation of Allergy occurs when pollinose, that is, contact with the pollen.
How to distinguish allergic rhinitis from cold
To distinguish allergic rhinitis from cold it is best to consult a specialist doctor.
Colds the common cold is infectious in nature, so it occurs on the background of hypothermia, SARS, bacterial infection. How to determine etiology – doctor knows.
The immune system fights off pathogens by increasing the body temperature. Usually allergic rhinitis rarely occurs with temperature rise, and it rises not more than 37 – 37.5 °C. When catarrhal rhinitis, the body temperature can rise to 38°C and above.
Also in infectious rhinitis signs of intoxication: malaise, weakness, drowsiness, loss of appetite, a small child – crying, moodiness, or Vice versa lethargy.
When bacterial rhinitis nasal discharge are in the nature of an opaque thick yellow or green discharge. In viral or allergic inflammation – watery liquid and transparent.
Usually infectious or catarrhal rhinitis passes for one or two weeks, which is not true about allergic. In continuous contact with the allergen the inflammation drags on for months or more, regardless of the time of year. Upon elimination of the allergen the symptoms of the disease are held for 1-2 days. It is usually noticeable when leaving on vacation in a different climate zone – stop contact with allergens and disease disappears.
In addition, the symptoms of allergic rhinitis go away after taking desensitizing drugs, which is not true of infectious disease.
Diagnosis and treatment of allergic rhinitis
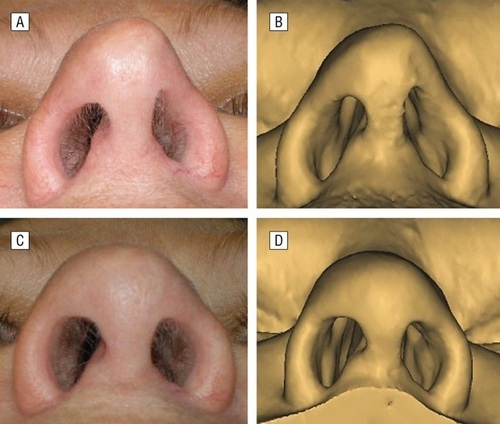
Diagnosis of allergic rhinitis includes mandatory visits to the doctor’s consultation with a visual inspection of the nasal passages with the help of special tools – rhinoscopy. In some cases, allergic rhinitis or accompanied by a disease of the Airways and the pneumatic sinuses. The doctor will see is characteristic of allergic inflammation of the mucous membrane swelling, redness, watery discharge in the nose.
Characteristic of allergic blood cells eosinophils normally do not detected in the nasal cavity. And in the presence of the described diseases are detected in two out of three patients suffering from allergic rhinitis. So smear on the eosinophils of the nasal cavity is taken for setting or confirmation of the diagnosis and greatly facilitates the diagnostic process. It does not require much cost and is quite easy.
Non-specific marker of Allergy is increasing the level of eosinophils in the blood. Therefore, each surveyed patients perform routine investigations: blood and urine tests. One out of three patients with allergic rhinitis eosinophilia is detected in the blood.
To clarify the nature of the disease of the consultation of the allergist. The doctor will examine skin samples to different types of allergens to determine the disease provoking agent. But research does not always lead to success. For testing procedures use a maximum of several hundred allergens, although in reality there are many more – tens of thousands. There are also some limitations for the conduct of skin samples: age from four to sixty years, the abolition of antihistamine medications at least 5 days before the study, contraindications to trial in pregnant, nursing and during the exacerbation of allergies.
In some cases confirm the presence of allergic process helps a blood test for immunoglobulins. In case of detection of high titers of immunoglobulin E can be suspected aggravation or manifestation of allergic disease. In some cases it is possible to undergo blood tests for specific antigens to specific antibodies. But these studies are expensive and often lead to false-positive results, therefore, are assigned very rarely.
Treatment of allergic rhinitis should not be underestimated. This is the key to a peaceful and proper work of the immune system, and therefore the potential health of the whole organism.
How to treat allergic rhinitis. Funds from allergic rhinitis
The question of how and what to treat allergic rhinitis or hay fever is the most complete answer specialists allergists. To assign adequate treatment the doctor needs to know the reasons, including specific allergens causing the illness, assess the severity of the symptoms and to exclude other diseases which may be accompanied by a runny nose.

In each case, the pathology cannot confidently say how you will proceed with the treatment. As a rule, it is selected and adjusted in accordance with medical recommendations individually, depending on effectiveness and nature of the disease.
In addition to treatment with medicines should be strictly follow the rules of hypoallergenic regime, which include contacts with potential allergens to a minimum. This includes the exclusion of foods with a high content of allergen (chocolate, oranges, seafood, preservatives and colorants), as often as possible, wet cleaning the house, removing the contact with plants and Pets, house sitting in flowering field plants.
There are two main types of treatment:
- General anti-inflammatory treatment
- therapy directed at a specific allergen, if you were able to find it
Primarily for suppression of allergic inflammation in the mucosa prescribe medicines that suppress the main mediator of allergic inflammation – histamine, which in large quantities is ejected from the immune cells in the mucosa. It antihistamines of different generations, preferably the third (“zyrtec”, “aerius”) or the second (“Kesten”, “tsentrin”, “claritin”). Treatment usually lasts at least two weeks but not constantly, as it can develop addiction. These drugs are taken orally in form of tablets or drops and affect the General mechanisms of Allergy.
The ineffectiveness of such treatment for therapy add drugs for local application: sodium cromoglicate (“chromosol”, “good cough medicine”), hormonal drugs in the form of aerosols (“nasonex”, “alderin”, “almost four years”, “binaryn”). They are appointed and chosen by the doctor individually and apply 1-2 times a day. Corticosteroids usually are most effective in the treatment of allergic rhinitis and included in the “gold standard” of therapy.
Usually the treatment of disease by means of allergic rhinitis is prolonged, not less than 2-4 months. During this time the immune system “calms down”, reduced hypersensitivity to foreign substances, and disappear the symptoms of allergic rhinitis reduces the chance of recurrence.



Your style is so unique compared to many other people. Thank you for publishing when you have the opportunity,Guess I will just make this bookmarked.
Right here is the right blog for everyone who would like to understand this topic. You realize a whole lot its almost tough to argue with you (not that I really would want to…HaHa). You definitely put a fresh spin on a topic which has been discussed for ages. Great stuff, just great.
I’m amazed, I must say. Rarely do I encounter a blog that’s both equally
educative and engaging, and without a doubt, you have hit the nail on the head.
The problem is something too few folks are speaking intelligently about.
Now i’m very happy I came across this during my search for something regarding
this.